
RESEARCH: AREAS OF INTEREST
Aging is the progressive increase of physiological deterioration leading to impaired organ function and is a primary risk for degenerative diseases. Aging is universal to all living species, and it has always been assumed that it is unavoidable. In recent years, however, the science of aging has demonstrated unequivocally that the development of aging is controlled by biomolecular and genetic pathways.
At the Center for Healthy Aging (CHA), we work on several areas of interest. These include:
Geroscience has exploded in recent years due to advances at Stony Brook and other institutions. For example, researchers at SBU are examining ways to control senescent cells (cells that deteriorate with age), which accumulate with age in various tissues and play a causal role in chronic diseases such as diabetes, cancer, osteoarthritis and Alzheimer’s disease.
SBU has considerable strengths in research into the biology of cellular senescence, the impact of endogenous viruses in mediating inflammatory pathways of senescent cells and in imaging inflammatory signaling and metabolic dysfunction within tissues. The CHA will support a vibrant program of geroscience research and is already leveraged by substantial federal funds. Convergence of existing expertise relating to aging, including DNA damage, endogenous retroviruses, inflammaging, immunology, metabolism and neurodegenerative diseases that are the main pillars of geroscience, will be the cornerstone of the CHA.
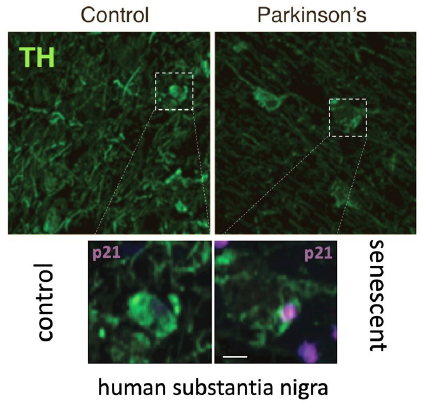
Microscope images of human brain showing increased p21 (in magenta), a marker for senescence, and decreased tyrosine hydroxylase (TH, in green) in patients with Parkinson’s disease compared to age-matched controls. Accumulation of senescent cells causes age-related inflammation, so-called “inflammaging,” and loss of nerve cells, which causes Parkinson’s disease. The discovery of this kind of “inflammaging” is novel in Parkinson’s and has potential for new therapeutic interventions to stop progression of the disease. (Images from Riessland et al., Cell Stem Cell, 2019).
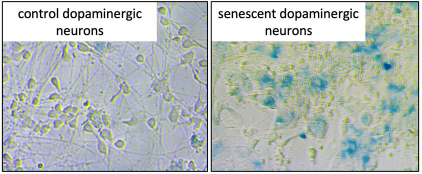
Images of human stem cell-derived dopaminergic neurons, the nerve cells that are affected in Parkinson’s disease. Blue staining positive cells are senescent neurons. The senescent cells on the right are cells that were depleted for the Parkinson’s risk gene SATB1. These data show that dopamine neurons are capable of entering a state of senescence which could lead to midbrain “inflammaging.” (Images from Russo [unpublished] and Riessland et al., Cell Stem Cell, 2019).
Stony Brook has unique imaging resources that will be a central focus of the CHA. Positron emission tomography (PET) is used to image and measure molecular targets of interest (e.g., markers of inflammation). Brain PET, in particular, is uniquely suited for aging research.
SBU has world-class PET imaging facilities, including two research dedicated PET scanners, a simultaneous PET/MRI and a preclinical PET imaging facility, allowing quantification of targets in rodents, non-human primates, and humans. The facility can synthesize PET tracers that target acetylcholine, amyloid, dopamine, glutamate, serotonin, metabolism and inflammation. Further, with experts in PET tracer development, the ability to design and synthesize new PET tracers to examine targets previously unseen in living people can be offered to CHA investigators.
Stony Brook is one of the few institutions in the world that can perform full quantification of these targets. With these services, a major goal for the CHA will be to expand the application of PET to aging research in the brain and other tissues.
The RSOM has a large geriatric clinical practice that includes ambulatory and inpatient services, outreach programs to nursing and rehabilitation centers in our area, including the Long Island State Veterans Home on the Stony Brook University campus, and a program on translational research and geriatric care.
The Center of Excellence for Alzheimer’s Disease serves more than 54,000 patients on Long Island suffering from Alzheimer’s disease and related dementias. In addition, Stony Brook Medicine has achieved designation as an Age-Friendly Health System by the Institute for Healthcare Improvement and is working to improve care related to geriatrics.
The Health Resources Services Administration awarded a $10 million grant to SBM to create inpatient research capacity. With these existing outstanding clinical programs, the CHA represents a unique opportunity for faculty to address the basic and clinical science of the multisystem decline of physiologic systems with aging; develop unique, interdisciplinary strategies to study our aging patients; and reach out to the community to develop services that will enhance the quality of life for older adults.
The science of mobility bas been identified as a new research opportunity that would be inclusive of our medical specialties, other schools of the Health Sciences and the university.
One example of an area that the CHA may focus on is the science of mobility. Mobility is an understudied area of science, disturbances of which lead to falls, the most common cause of injury and a leading cause of morbidity and mortality in the aging. The science of mobility builds on existing SBU strengths in neurodegeneration, metabolism, biomedical engineering and population health, and provides an opportunity to expand research in fields such as orthopaedics and ophthalmology.
Mobility science encompasses many medical and surgical specialties, all Health Sciences Schools, and the Stony Brook University campus. An integrated, multidisciplinary approach to understanding factors that contribute to reduced mobility may help to target interventional strategies or environmental modifications to reduce the occurrence of falls (Figure 1 – Multidisciplinary Aging Research). The theme of mobility is ideal for population-based studies and for extending our clinical research to older patients in their own homes.
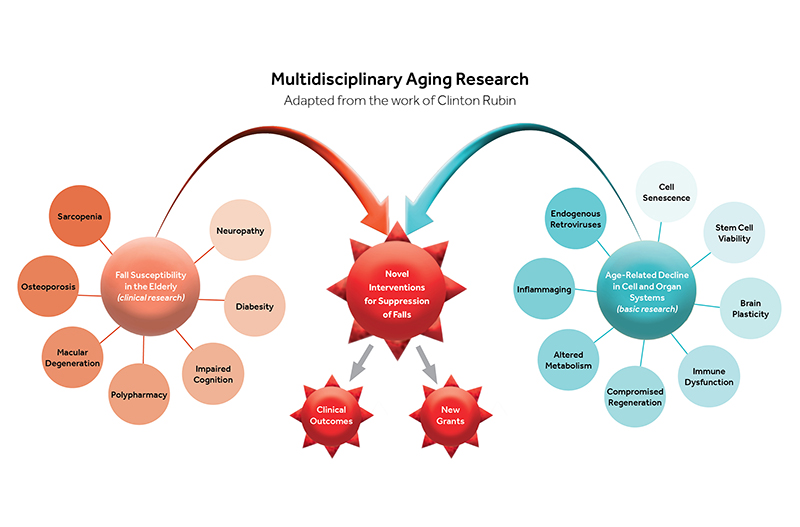
With age, diseases such as macular degeneration, diabetic neuropathy, osteoporosis and sarcopenia, as well as age-related declines in hearing, diminish the quality of the integrated sensory input systems that are critical to stability. Neurodegenerative diseases, such as Alzheimer’s and Parkinson’s undermine the ability to perceive, process and respond to environmental cues, increasing fall risk. Fall risk is a complex amalgam of many different system inputs that will involve geriatrics, orthopedics, ophthalmology, neurology, radiology, lifestyle medicine, nutrition and nursing. Stony Brook’s research endeavors, focusing on reducing age-related decline/disease through multidisciplinary approaches will result in a reduction of falls.
The CHA represents an unprecedented continuum of research and patient care. The combination of these unique assets will help formulate a one-of-a kind academic partnership that will offer education and training opportunities leading to increased competitiveness for additional federal and state funding, synergize with the Long Island Network for Clinical and Translational Science (LINCATS) , and provide a competitive edge for Program Project Grants at the National Institute on Aging (NIA).
RESOURCES ON AGING
Older Adults Outnumber Children in 11 States and Nearly Half of U.S. Counties
United States Census Bureau
The U.S. population age 65 and older rose by 3.1% (to 61.2 million) while the population under age 18 decreased by 0.2% (to 73.1 million) from 2023 to 2024, according to the Vintage 2024 Population Estimates released today by the U.S. Census Bureau. READ MORE
The 5Ts Framework
National Institutes of Health
The 5Ts Framework helps research teams identify the appropriate target population and avoid exclusions, build teams with aging expertise, anticipate additional time and resources needed, follow practical tips for accommodating age-related limitations, and use tools that measure outcomes important to older adults. READ MORE
AGS|AGING Learning Collaborative
AGS|AGING|Multiple Chronic Conditions Research
The AGS/AGING Learning, Educating, And, Researching National Initiative in Geriatrics ("LEARNING") Collaborative, an R25 grant from the National Institute on Aging (NIA), has been awarded to the American Geriatrics Society in partnership with the Health Care Systems Research Network (HCSRN)-Older Americans Independence Centers (OAICs) AGING (Advancing Geriatrics Infrastructure and Network Growth) Initiative. The Collaborative aims to fill educational and training gaps in multiple chronic conditions (MCCs) research. READ MORE
Tap Into A Rich Repository of Biospecimens and Data for Aging Research
National Institutes of Health
Did you know that valuable data and biosamples from aging studies may help accelerate your current investigations? To assist, NIA continues to expand its Aging Research Biobank, a state-of-the-art inventory of biological specimens and phenotypic, clinical, and imaging data from decades of our institute’s funded studies. READ MORE
Research in Context: Can we slow aging?
National Institutes of Health / NIH Research Matters
Aging is a leading cause of disease and disability. This special Research in Context feature explores research into the biology of aging, including how to measure its speed and progression and ways it might be slowed down or even reversed. READ MORE