|
Assistant Professor Department of Microbiology and Immunology Ph.D., Microbiology and Immunology, University of Miami, 2014 |
|
|
E-mail: |
Priyadharshini.Devarajan@stonybrook.edu |
|
|
Research |
We study the basics behind successful immunity against respiratory infections. In particular, we study memory T and B responses that are reactivated upon infection in the lung and the nose, to protect against severe disease. Nasal Immunity T cell responses resident in the respiratory tract provide a first line of defense against respiratory infections. Airborne respiratory pathogens infect the nasal mucosa before infecting the lungs. Clearing most virus before it replicates and spreads to the lung is the key to sterilizing immunity. However, the role of immune responses within the nasal tissue are remarkably unexplored. Most studies on respiratory tissue immunity have focused on responses in the lung, even though strong lung immune responses often come at the cost of lung tissue damage. We study whether having powerful immune responses in your nose make you less vulnerable to severe cases of respiratory infections. This insight could lead to the development of superior vaccines that not only reduce illness severity but also curb virus transmission.
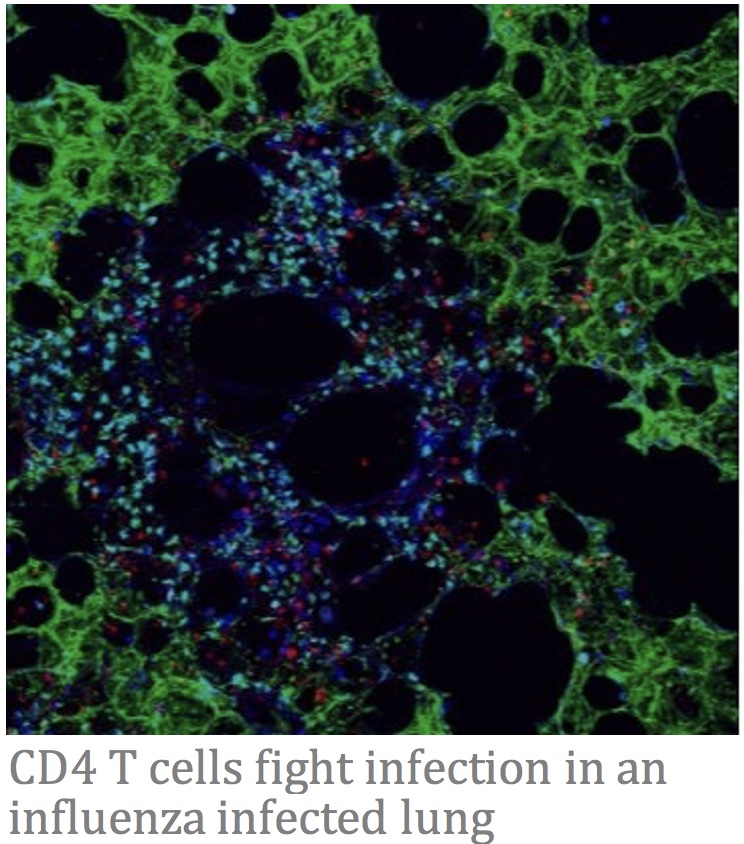
Origin of Lung T cell Memory T cell responses are an arm of the immune response that target internal proteins of viruses/bacteria that are less likely to mutate (because they are usually important for replication machinery). Immune memory based on T cells can provide us long-lived stable protection against pathogens which mutate every season like influenza or SARS CoV2. Memory T cells in the infected tissue are amongst the first responders combatting infection and are called tissue-resident memory T cells (Trm). Thus, effective vaccines must induce robust and durable lung Trm to provide optimum long-term protection against respiratory infections. In this project, we aim to identify the effector T cell precursors that differentiate into protective lung Trm. Uncovering Immune Responses that Function Optimally in Elderly Individuals.
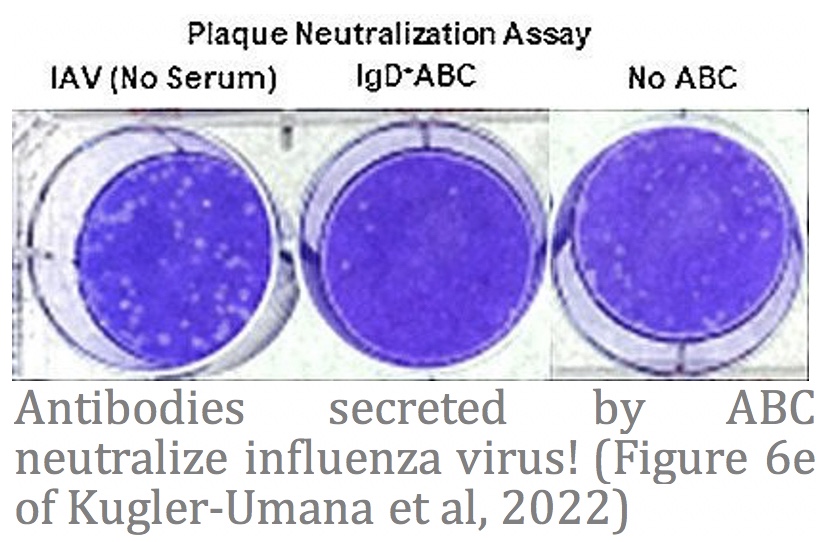
Naïve conventional B and T cells decline and become poorly responsive with age making the elderly highly susceptible to severe disease and death when exposed to new pathogens, like new strains of influenza or SARS-CoV2. This phenomenon also underlies current poor efficacies of vaccines in the aged. However, our recent studies discovered that an arm of B cell responses, called Age-associated B cells (ABC) are absent in the young but develop with age and are specialized to respond to pathogens in an aging immune environment. ABC could be targeted with vaccines to induce effective protection in the aged against pathogens. We study these ABC responses and aim to understand how they can be induced to be the most protective, with a special focus on their protective ability against respiratory infections.
|
|
| Publications |
Selected Publications: Devarajan P#, Vong AM, Castonguay CH, Silverstein NJ, Kugler-Umana O, Bautista BL, Kelly KA, Luban J, Swain SL#. 2023. Cytotoxic CD4 Development Requires CD4 Effectors to Concurrently Recognize Local Antigen and Encounter Infection-Induced IL-15. Cell Reports. 42 (10). #Co-corresponding author Kugler-Umana O, Zhang W, Kuang Y, Liang J, Castonguay CH, Tonkonogy SL, Marshak-Rothstein A, Devarajan P#, Swain, SL#. 2022. IgD+ Age-Associated B cells are the progenitors of the main T-independent B cell response to infection that generates protective Ab and can be induced by an inactivated vaccine in the aged. Aging Cell. e13705. #Co-corresponding authors Devarajan P, Bautista B, Vong AM, McKinstry KK, Strutt TM, Swain SL. 2016. New Insights into the Generation of CD4 Memory May Shape Future Vaccine Strategies for Influenza. Frontiers in Immunology. 7(April), 1–7. |
|