Research
Dr. Speer’s Laboratory in the Division of Neonatology of Stony Brook Children’s Hospital focuses on the immunopathology of neonatal sepsis and inflammation and the development of adjunctive anti-inflammatory pharmacological therapies that can improve survival and outcome of infected newborns. The Lab especially aims to identify ways to control the effects of central nervous system inflammation on the developing neonatal brain.
Current active projects are:
 Human in vitro cord blood model for the screening and study of mechanisms of action of candidate adjunctive anti-inflammatory pharmacological agents for newborn sepsis and the identification of novel synergistic combinations of anti-inflammatory drug therapies.
Human in vitro cord blood model for the screening and study of mechanisms of action of candidate adjunctive anti-inflammatory pharmacological agents for newborn sepsis and the identification of novel synergistic combinations of anti-inflammatory drug therapies.- Neonatal bacterial sepsis murine models for pre-clinical testing of adjunctive anti-inflammatory therapies. These models are particularly aimed to investigate the acute and delayed effects of newborn infections and of anti-inflammatory treatments on neurodevelopmental outcome.
The lab uses the following special techniques:

H&E-stained sections of PN7 kidneys in murine sepsis In vitro drug screening methods for anti-inflammatory drug responses based on whole blood, isolated immune cells, and tissues
- Flow cytometry, multiplex immunoassays, Western blotting, qRT PCR, microbiological assays, microarray, and proteomics
- In vitro and in vivo use of neonatal live pathogenic microorganisms
- Conventional and confocal microscopy
- Optical imaging of bacterial infections in newborn rodents
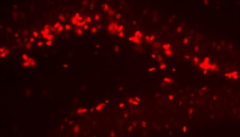
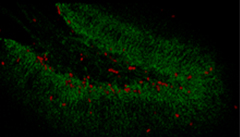
- Nucleotide analogues to study the effects of murine neonatal neuroinflammation on neurogenesis and developmental outcome
 |  |  |
|---|---|---|
| BrdU, 20X, hippocampal section, PN14 | BrdU 647, DCX 488, hippocampus, PN14 | Speer at al., Antimicrob Agents & Chemother 2018 |
Faculty and Staff
 Esther Speer, MD, Associate Professor of Pediatrics, is the principal investigator of the laboratory. She graduated from Johannes Gutenberg University in Mainz Germany, and completed her doctoral thesis (equivalent to PhD) at the Rheinische Friedrich-Wilhelms University in Bonn Germany. Her clinical training consisted of pediatric residency training at the State University of New York at Brooklyn, followed by a neonatal-perinatal fellowship at the University of Pittsburgh and the University of Chicago. As a neonatology physician scientist at Stony Brook Children’s Hospital, Dr. Speer also treats newborn patients admitted to the Neonatal Intensive Care Unit, including neonates with sepsis and other severe infections. Her research focuses on the immune-pathological mechanisms of newborn sepsis and the pharmacological control of infection-induced hyperinflammation in the term and preterm neonate. Her lab employs in vitro and in vivo models of neonatal bacterial infections to study the impact of microbe-induced inflammation on neonatal outcome, including the effects of neuroinflammation on the developing brain and its responses to immune-modulatory pharmacological interventions.
Esther Speer, MD, Associate Professor of Pediatrics, is the principal investigator of the laboratory. She graduated from Johannes Gutenberg University in Mainz Germany, and completed her doctoral thesis (equivalent to PhD) at the Rheinische Friedrich-Wilhelms University in Bonn Germany. Her clinical training consisted of pediatric residency training at the State University of New York at Brooklyn, followed by a neonatal-perinatal fellowship at the University of Pittsburgh and the University of Chicago. As a neonatology physician scientist at Stony Brook Children’s Hospital, Dr. Speer also treats newborn patients admitted to the Neonatal Intensive Care Unit, including neonates with sepsis and other severe infections. Her research focuses on the immune-pathological mechanisms of newborn sepsis and the pharmacological control of infection-induced hyperinflammation in the term and preterm neonate. Her lab employs in vitro and in vivo models of neonatal bacterial infections to study the impact of microbe-induced inflammation on neonatal outcome, including the effects of neuroinflammation on the developing brain and its responses to immune-modulatory pharmacological interventions.
Current Collaborators at Stony Brook University
- Bettina Fries, MD, FIDSA, Professor, Chief of Division of Infectious Diseases, Department of Medicine
- Helen Hsieh, MD, PhD, Assistant Professor, Division of Pediatric Surgery, Department of Surgery
- Grigori Enikolopov, PhD, Professor, Department of Anesthesiology
- Sheed Itaman, PhD Candidate, Department of Neurobiology and Behavior
- Robert Woronicki, MD, MS, Div. Chief of Pediatric Nephrology & Hypertension, Department of Pediatrics
- Nicholas Carpino, PhD, Associate Professor, Department of Microbiology and Immunology
Current Funding
NIH NIAID - R21 AI149296-01 (PI Speer)
National Institute of Allergy and Infectious Diseases
Immunomodulatory therapy to improve outcomes of neonatal sepsis
Goal: Characterization of the effects of Pentoxifylline on systemic and cerebral cytokine and chemokine responses in a term and preterm murine model of neonatal sepsis. Exploration of the feasibility and sensitivity of in vivo PET imaging as a non-invasive tool to study brain involvement in systemic bacterial infections and response to therapies in neonatal rodents.
Targeted Research Opportunities Fusion Award (PI Speer)
Renaissance School of Medicine at Stony Brook University
Early and delayed neurological effects of newborn sepsis
Goal: Investigation of the acute and delayed neurological effects of bacterial sepsis and of sterile inflammation and their modulation with anti-inflammatory therapy, and subsequent hippocampal neurogenesis, cognition and behavior in newborn, infant and weaning mice.
Department of Pediatrics Intramural Grant (PI Speer)
Stony Brook University & Stony Brook Children’s Hospital
Anti-inflammatory therapy in a newborn mice sepsis model
Goal: Characterization of the synergistic effects and mode of action of combinations of anti-inflammatory agents in a preterm and term newborn mouse model of bacterial sepsis.
Recent Publications
- Speer EM, Diago-Navarro E, Ozog LS, Raheel M, Levy O, Fries BC. A neonatal murine Escherichia coli sepsis model demonstrates that adjunctive pentoxifylline enhances the ratio of anti- vs. pro-inflammatory cytokines in blood and organ tissues. Frontiers in Immunology, 2020; 11:577878. PMID: 33072121.
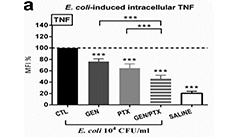
- Speer EM, Diago Navarro E, Ozog LS, Dowling DJ, Huo W, Raheel M, Fries BC, Levy O. Pentoxifylline alone or in combination with gentamicin or vancomycin inhibits live microbe-induced pro-inflammatory cytokine production in human cord blood and cord blood monocytes in vitro. Antimicrobial Agents and Chemotherapy. 2018, 62: e01462-18. PMID: 30275087.
- Speer EM, Dowling DJ, Xu J, Ozog LS, Mathew JA, Chander A, Yin D, Levy O. Pentoxifylline, dexamethasone and azithromycin demonstrate distinct age-dependent and synergistic inhibition of TLR- and inflammasome-mediated cytokine production in human newborn and adult blood in vitro. PLoS One. 2018, 13: e0196352. PMID: 29715306.
- EM Speer, X Lin, A Murthy, W Hou, S Islam, N Hanna. Pentoxifylline inhibits lipopolysaccharide-induced inflammatory mediators in human second trimester placenta explants. Placenta. 2017; 58: 60-66. PMID: 28962697.
- Speer EM, Dowling DJ, Ozog LS, Xu J, Yang J, Kennady G, Levy O. Pentoxifylline inhibits TLR- and inflammasome-mediated in vitro inflammatory cytokine production in human blood with greater efficacy and potency in newborns. Pediatric Research. 2017; 81: 806-816. PMID: 28072760.
For a complete list of publications:
https://www.ncbi.nlm.nih.gov/myncbi/1HyrspwtpQX/bibliography/public/
Announcements
- Undergraduate students interested in developmental immunology, microbiology or neurobiology research are welcome to join our lab to gain research experience, which they may also apply for credit as part of their degree. Any student interested in our laboratory research experience may contact the PI by email and submit their CV and personal statement.
- Medical residents and fellows interested in translational or basic science research related to neonatal immunology and infectious diseases, microbiology, or developmental biology are encouraged to contact the PI and inquire about current research opportunities for medical trainees in our lab.
- Positions for postdoctoral associates in microbiology, immunology, neurobiology, developmental biology, or related fields become periodically available, and are posted on the Talent Management System of Stony Brook University and other sites. Interested researchers may contact the PI by email for any inquiries.
Important Dates and Events
- Pediatric Resident Research Fair, October 20th, 2021
- Annual Pediatric Research Day, May 25th, 2022
- Pediatric Academic Societies Annual meeting, April 21st to 25th, 2022, Denver, CO (Our lab regularly attends this meeting.)
Contact Information
Email: Esther.Speer@stonybrookmedicine.edu
100 Nicolls Road, Health Science Center Level 11, Department of Pediatrics, Stony Brook, NY