
Salvatore Docimo Jr., DO, MS, of our Bariatric, Foregut, and Advanced Gastrointestinal Surgery Division, has just performed Suffolk County's first per-oral pyloromyotomy (POP) — a novel, minimally invasive procedure to treat gastroparesis.
The POP procedure, also known as G-POEM that stands for gastric per-oral endoscopic myotomy, is a newly developed treatment offering patients attractive benefits, compared with other surgical therapies for gastroparesis.
Gastroparesis, or delayed gastric emptying, is a stomach disorder in which food moves through the stomach into the intestines slower than normal. (The etymology of "gastroparesis" is: gastro- from ancient Greek γαστήρ gaster, "stomach" and πάρεσις -paresis, "partial paralysis.")
Patients often experience chronic nausea, vomiting, bloating, feeling full too soon after starting to eat, and weight loss. It is a debilitating condition, at times requiring hospitalization, and can significantly affect a person's quality of life.
Common causes include diabetes and previous surgery. Diabetes has been noted to be a cause in 30% of gastroparesis cases. However, neurological disease, collagen vascular disorders, viral infection, and drugs have all been blamed.
POP is a novel, minimally invasive procedure at the forefront of gastroparesis treatment.
Gastroparesis is believed to occur in 9.6 per 100,000 people in men and 37.8 per 100,000 people in women. A recent study has also demonstrated an increase in gastroparesis-related hospital admissions by nearly 300% over a 16-year period.
"POP is a novel, minimally invasive procedure that is at the forefront of gastroparesis treatment. We are excited to offer the POP procedure as an option for our patients," says Dr. Docimo.
Gastroparesis may result in the following complications, which, in addition to potentially problematic symptoms, justify treatment:
- Severe dehydration: This condition is due to chronic vomiting.
- Malnutrition: Patients tend to have poor appetites and cannot meet their daily caloric requirements.
- Poor glucose control: Poor control over the amount and rate of food passing from the stomach to the small bowel can cause poorly controlled blood sugar levels.
- Poor quality of life: Symptoms can make it difficult to maintain a normal quality of life and may affect a patient's work and social life.
Surgical treatment options for gastroparesis are reserved for patients with symptoms that have not responded well to lifestyle/dietary modifications and medical management.
The surgical options include implantation of a gastric electrical stimulator, placement of feeding tubes, pyloroplasty (open or laparoscopic), total gastrectomy (removal of the stomach), and the POP procedure
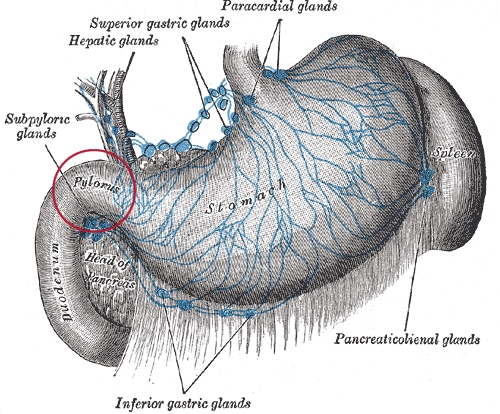
| The stomach showing location of pylorus (red circle); source, Henry Gray's Anatomy of the Human Body (1918). (Click on image to enlarge.) |
POP is the most minimally invasive surgical option, using an endoscope (thin flexible tube). It is an alternative to more conventional pyloroplasty, in which the pylorus — a disc-shaped muscle that allows emptying of the stomach — is cut.
The cutting of this muscle aims to improve passage of food contents from the stomach into the small intestine.
With POP, there generally are no incisions made on the body, as everything is done through an endoscope that is passed through the mouth, into the esophagus, and down into the stomach.
The physician uses a small knife at the tip of the endoscope to create a tunnel to the pylorus, which is then cut, and the tunnel is closed.
The POP procedure offers an option for patients who need to avoid the problems associated with surgery. Most patients will be in the hospital for one day and require a post-procedural upper gastrointestinal study to ensure the effectiveness of the procedure.
| The newly established Stony Brook Gastroparesis Center, under the direction of Dr. Salvatore Docimo Jr., offers a multidisciplinary approach that brings together experts in the areas of surgery, gastroenterology, psychology, and nutrition. The center's goal is to provide patients with digestive disorders, especially gastroparesis, a wide spectrum of diagnostic and treatment options under one roof. |
