Our outpatient clinic offers expertise in infections acquired overseas in returning travelers.
Babesiosis
Long Island is the epicenter of tick borne diseases, and Babesiosis, caused by the parasite Babesia microti, is the most common parasitic disease in this region. Suffolk County reports every year the highest absolute number of Babesia cases in NY state, with 153 in 2016 (1). At SBUH, we have observed an steady increase in the number of hospitalized cases per year with babesiosis from 1 in 2008 to 16 in 2014 (2).
The main route to acquire this infection is by a bite from a black legged tick (Ixodes scapularis) during the warm months. This particular tick also transmits Borrelia burgdorferi, the agent that causes Lyme disease. Most people who acquired babesiosis do not have symptoms and therefore do not need treatment. Before considering treatment, it is highly recommended to make sure the diagnosis is correct.
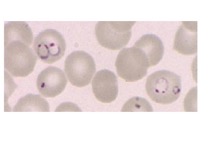
Patients who tested positive for IgG-Babesia in a blood test may indicate an old infection, and not necessarily a current infection. In the acute disease, multiple blood smears are usually positive for the parasite (see below). Risk factors for developing severe disease are people without spleen (asplenia), advanced age and those with immunosuppression (HIV, corticosteroid therapy, malignancy) and, on these particular patients, treatment should be individualized.

Ring-shaped of Babesia parasites inside a red blood cell.
Chagas Disease
Chagas disease is a parasitic infection caused by Trypanosoma cruzi that affects approximately 8-10 million Central and South Americans. Most infected people are without symptoms for decades before developing organ dysfunction. After 2-3 decades with the infection, about 20-30% of people will progress to develop cardiac disease including heart failure, strokes, and sudden death from arrhythmias or gastrointestinal dysfunction. Only two drugs (benznidazole and nifurtimox) are currently available to treat T. cruzi infection. Of these, only benznidazole is approved by the FDA for use in children 2–12 years of age (3). It is commercially available at http://www.benznidazoletablets.com/en/. We specialize in the treatment for Chagas disease (4). A positive test for Chagas does not confirm the diagnosis. We have experienced in confirming the diagnosis with CDC assistance. Treatment should be individualized.
Malaria
Millions of domestic and international visitors arrive to New York every year and many U.S. citizens travel overseas. Travelers may acquire parasitic infections anywhere in the world, and the most common parasitic infection acquired overseas by U.S. travelers is malaria, caused by Plasmodium species. When traveling to endemic areas, preventative treatment against malaria is strongly recommended. We also evaluate and manage patients with fevers after a travelling to the tropics.
Ring forms of Plasmodium in red blood cells in a traveler returning from Africa.
Neurocysticercosis
This is a parasitic infection caused by larvae of the helminth Taenia solium. It can cause seizures, and thus most cases are diagnosed post-seizure in the emergency department of a hospital. This infection is most commonly present in low-income countries, but cases can also be found in the U.S. Treatment varies according to the stage of the disease (5). At SBUH, at least 44 cases have been diagnosed in the last few years. [SBUH study on Neurocysticercosis: https://academic.oup.com/ofid/article/3/suppl_1/584/2636956].
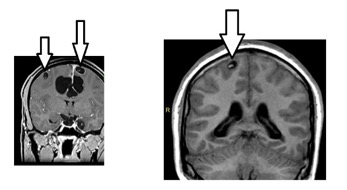
Multiple vesicular phase cysts with scolex (arrows). No edema in surrounding parenchyma.
Global Health Institute of Stony Brook University
In addition to our local research, we are studying Parasitic Diseases in Madagascar and Peru in collaboration with the Global Health Institute of Stony Brook University. [http://www.stonybrook.edu/commcms/ghi/projects/parasites.php].
Contact us: If you are interested in an appointment with our outpatient facility, please have your doctor’s office fax their last progress report along with your blood work to 631-444-7518.
References
1. New York State Department of Health, 2016. Available at https://www.health.ny.gov/statistics/diseases/communicable/2016/docs/cases.pdf
2. Kletsova EA, Spitzer ED, Fries BC, Marcos LA. Babesiosis in Long Island: review of 62 cases focusing on treatment with azithromycin and atovaquone. Ann Clin Microbiol Antimicrob. 2017;16(1):26. doi: 10.1186/s12941-017-0198-9
3. CDC, 2018. Available at https://www.cdc.gov/parasites/chagas/health_professionals/tx.html
4. Bern C, Montgomery SP, Herwaldt BL, et al. Evaluation and Treatment of Chagas Disease in the United States: A Systematic Review. JAMA, 2007; 298(18):2171–2181. doi:10.1001/jama.298.18.2171
5. White AC, Coyle CM, Rajshekhar V, Singh G, Hauser WA, Garcia HH, Nash TE, Diagnosis and Treatment of Neurocysticercosis: 2017 Clinical Practice Guidelines by the Infectious Diseases Society of America (IDSA) and the American Society of Tropical Medicine and Hygiene (ASTMH), Clin Infect Dis 2018; 66(8): e49–e75, https://doi.org/10.1093/cid/cix1084
Additional information
For travelers: https://wwwnc.cdc.gov/travel/
Parasites acquired overseas: https://www.cdc.gov/parasites/travelers.html
General information: https://www.cdc.gov/parasites/index.html
Chagas en español https://www.cdc.gov/parasites/chagas/resources/es/informativa_breve.pdf