Our categorical internal medicine training program is designed to provide a comprehensive experience in internal medicine. Residents are exposed to a wide variety of clinical experiences in acute and ambulatory medicine. Our clinical curriculum emphasizes the breadth and depth of internal medicine and offers a broad choice of electives to support each resident's unique clinical and research interests.
Highlights of Some of Our Unique Rotations
Leukemia/Lymphoma and Bone Marrow Transplant Elective
In addition to our required medical oncology rotation where our residents manage complications of solid tumors and chemotherapy, our residents care for high acuity bone marrow transplant patients on our Leukemia, Lymphoma, Transplant (LLT service) elective. Residents can also participate in outpatient elective rotations in the Stony Brook Cancer Center, which has been recognized as one of the first and largest cancer centers on Long Island. The clinical opportunities to care for both solid and liquid tumors ensure a robust clinical education in hematology and oncology.
Ultrasound Education
The Internal Medicine Residency program at Stony Brook maintains a tradition of providing a robust ultrasound curriculum. This curriculum is taught under the direction of our Pulmonary/Critical Care Medicine Faculty and mirrors the training given to our Pulmonary/Critical Care Fellows during their advanced education. During simulation on every Academic Wednesday, residents are instructed to use ultrasound and echo simulators for diagnosis and management of respiratory failure, shock, and abdominal pain. Additionally, residents are instructed on the use of POCUS (point-of-care ultrasound) with procedure simulation exercises. On the wards and in the critical care units, residents have over ten machines available to them to use in their daily practice. Additionally, we offer ultrasound electives including "Introduction to Bedside Ultrasound" and "Ultrasound-Procedure."
Palliative Care Selective Rotation
Learning to effectively and empathically deliver bad news and guide patients and their families through care-planning decisions is an essential skill that we emphasize for all of our residents. We believe that early acquisition of these important skills improves confidence and competence in end-of-life care. During PGY2, every resident participates in our Palliative Care Selective, working directly with our Palliative Care Team to better understand pain management and effective strategies to conducting goals of care discussions and family meetings.
Renal Rotation (Team R)
Although our general medicine population exposes our residents to a wide array of renal pathology, we believe that a dedicated nephrology service that focuses on our dialysis and transplant population offers residents a unique opportunity to work one-on-one with our nephrologists and transplant faculty members. Our Team R rotation provides our residents exposure to a broad spectrum of renal diseases and renal replacement therapies and in-depth engagement in a dedicated service that provides care for renal transplant patients. Our residents are active participants in the variety of basic, translational, and clinical research conducted by the Division of Nephrology and Hypertension.
Cardiac Acute Care (CACU) and Coronary Care Unit (CCU) Rotation
During these rotations, interns work alongside a senior resident, a cardiology fellow, and a cardiology attending in a fast-paced environment where chest pain, heart failure, and arrhythmias are diagnosed, evaluated, and treated. Interns quickly become proficient in interpreting EKGs and in managing cardiac emergencies and heart failure exacerbations. Our PGY2 residents manage patients with advanced heart failure on devices such as Intra-Aortic balloon pumps, Impellas, and Left Ventricular Assist Devices in the CCU.
Medical ICU Rotation and Team Structure
Critical care education is a crucial aspect of residency training. Our 20-bed MICU is divided into two teams, each consisting of three interns, one senior resident, one pulmonary fellow, and one attending caring for a maximum of ten critical care patients per team. During this rotation, interns refine their bedside ultrasound skills (taught during Academic Wednesday Simulation) and perform procedures including midlines, central lines, paracenteses, and thoracenteses, all while learning how to care for critically ill patients in a closed ICU environment. Keeping each team to a 10-patient maximum allows our residents to focus on the complex presentations and pathologies they encounter and dedicated time to discuss cases in depth with consultants and perform procedures.
Electives are both inpatient and outpatient
We offer a large selection of sub-specialty electives in both the inpatient and outpatient settings. Our medical centers have inpatient and outpatient teams for all medicine subspecialties including allergy/immunology, cardiology, endocrinology, gastroenterology, geriatrics, infectious disease, hematology/oncology, nephrology, pulmonary, and rheumatology. We also offer unique experiences with our interdisciplinary teams, such as wound care, dermatology, sports medicine, LGBTQ+ care, weight management, mental health, and radiology. These rotations allow our residents to gain a well-rounded breadth of knowledge and experience and provides one-to-one clinical opportunities with attending physicians early on in training. As part of the 4+1 system, residents attend continuity clinic and participate in outpatient addiction medicine and hospice during their ambulatory week. The variety of elective offerings helps residents who are interested in pursuing a subspecialty form connections early in their residency training.
Intern Medical Admitting Night (IMAN) Rotation
IMAN is a dedicated admitting rotation for our interns. It’s based on a “big sibling” model in which our interns are paired with a senior resident on night float. The rotation provides extra support and guidance during the PGY1 year while the interns are still learning how to develop comprehensive management plans for their patients. This rotation mirrors the usual admitting night rotation with extra support to the interns. Close supervision and coaching are done by senior residents as well as dedicated in-house nocturnist attendings. The number of admissions is also lowered to allow our interns plenty of time at the bedside and to conduct point of care reading.
General Medicine Rotation – Geographic Allocation of Patients
On the General Medicine service, interns provide care for patients from diverse backgrounds with interesting disease processes. They work closely in an interdisciplinary team environment to ensure that patients are receiving the care and services they need while in and out of the hospital. At both Stony Brook University Hospital and the Northport VAMC, all of the general medicine teams are geographically co-located on the same unit/floor. The geographic model is not only convenient for the residents but also creates close collaboration with our nursing and social work/care management staff. Teaching rounds are heavily focused on clinical reasoning and resident autonomy with an emphasis on resident driven rounds in which the resident’s/intern’s role is the primary provider for the patient.
Medicine Admitting Resident (MAR)
The Medical Admitting Resident (MAR) rotation allows third year residents to position themselves as the first point of contact for critical care consults in the emergency room. The PGY3s conduct stabilization of the acutely ill patient, generate a diagnostic workup and treatment plan for critically ill patients and work directly with the critical care fellows and attendings for care and disposition of the patient. The MAR also directs medical admissions for the teaching teams – this ensures an enriched selection of teaching cases for the resident teaching teams. Our senior residents role model their well-honed communication, leadership, and clinical skills as MAR. The MAR works alongside our Medical Admitting Hospitalist whose role is to maintain bedboard and distribute admissions to the medicine services.
Categorical Curriculum
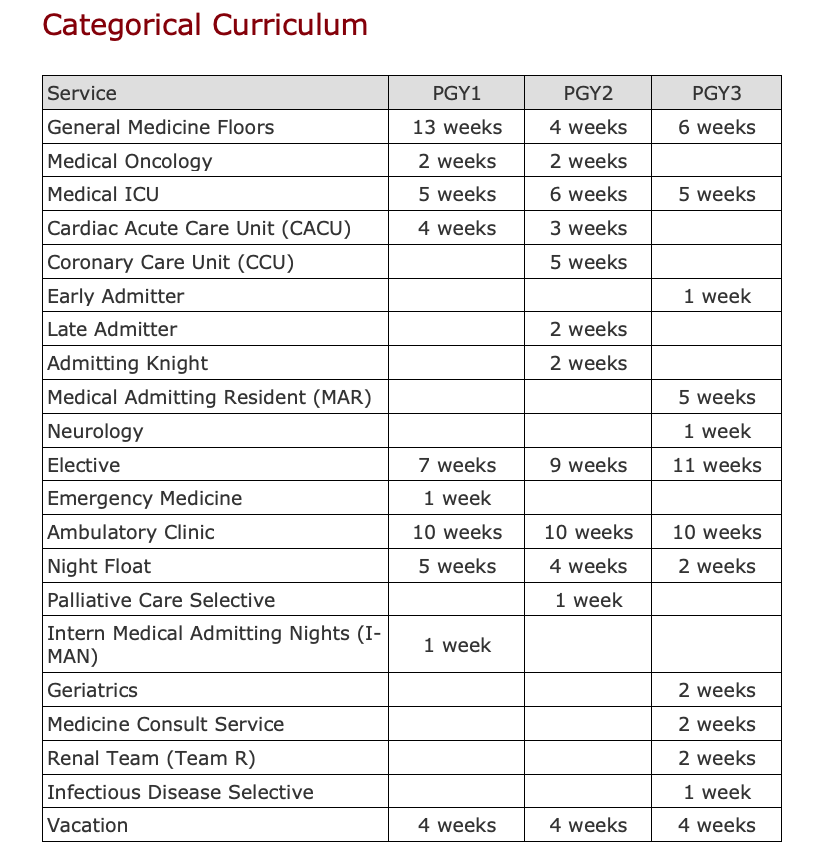
PGY 1 - Focuses on building exposure to a wide array of practice environments
The Intern year is strategically designed to provide interns exposure to both general medicine and a wide selection of subspecialty areas early on in training. The bulk of the rotations are focused on experiences in Cardiology (Coronary Artery Disease Cardiac Acute Care Unit (CACU), Pulmonary/Critical Care, Medical Oncology, General Medicine, Ambulatory Medicine, a mix of inpatient and outpatient electives, and a dedicated admitting Intern Medicine Admitting Nights (IMAN) rotation.
Intern year is divided into approximately 6 months of medicine floors (which includes General Medicine, and dedicated services for Coronary Artery Disease Cardiac Acute Care Unit (CACU), and Medical Oncology services), 10 weeks of outpatient continuity clinic, 7 weeks of inpatient and outpatient electives and 6 weeks of Medical Intensive Care Unit (MICU).
On the General Medicine service, interns provide care for patients from diverse backgrounds with interesting disease processes. They work closely in an interdisciplinary team environment to ensure that patients are receiving the care and services they need while in and out of the hospital. At both Stony Brook University Hospital and the Northport VAMC, all of the general medicine teams are geographically located together on the same unit/floor.
The dedicated Medical Oncology service is where interns learn to manage complications of solid tumors and chemotherapy as well as the importance of palliative care.
During the Cardiac Acute Care Unit (CACU) rotations, interns work alongside a senior resident, a cardiology fellow, and a cardiology attending in a fast-paced environment where chest pain, heart failure, and arrhythmias are diagnosed, evaluated, and treated. Interns quickly become proficient in interpreting EKGs and in managing cardiac emergencies and heart failure.
Our 20-bed MICU has two teams, each consisting of three interns, one senior resident, one pulmonary fellow, and one attending caring for a maximum of ten critical care patients per team. During this rotation, interns are able to refine their bedside ultrasound skills (which they learn during dedicated ultrasound courses on Academic Wednesdays) and perform procedures such as central lines, midlines, paracenteses, thoracenteses and lumbar punctures, all while learning how to care for critically ill patients in a closed ICU environment. Our interns participate in a hospice experience once weekly during their ambulatory week in the second half of the year.
We offer a large selection of electives in both the inpatient and outpatient setting which allows interns to gain a well-rounded breadth of knowledge and experience early on in training. Our variety of electives helps interns who are interested in pursuing a subspecialty form connections early in their residency training.
PGY 2 - Focus on becoming a leader and mentor
During the second year of residency, residents now use all the skills and knowledge they gained as interns to take on the senior resident roles of leaders and mentors on their teams. Residents manage, teach, and lead a team of interns and medical students on the general medicine floors, including the dedicated subspecialty services. To further refine clinical decision-making skills and promote autonomy, second year residents admit their own patients and formulate individualized assessments and plans for each patient. This principle carries over into the ICU setting as two second year residents care for critically ill veterans in our VA ICU alongside a pulmonary fellow and attending as well as in our cardiac ICU (CCU) alongside a cardiology fellow and attending. In these critical settings, residents are able to exercise the acute care and ultrasound skills they learned as interns in a more autonomous fashion while performing both new and previously learned procedures. Every PGY2 completes the Palliative Care Selective; working directly with our Palliative Care Team they learn how to effectively and empathically deliver bad news and lead family meetings, and guide patients through care-planning decisions. During the ambulatory week, PGY2s have an outpatient experience in addiction medicine.
PGY 3 - It all comes together! Getting ready for independent practice
The third year of residency is where it all comes together! Leadership, mentorship, and clinical skills are perfected and exercised daily to prepare residents for fellowship and attending duties upon graduation. Residents have a significant amount of autonomy and take on the role of junior attending on the medical floors making clinical decisions with oversight by an attending. This year offers unique exposure to geriatric and neurology rotations, nephrology and infectious disease rotations, a medicine consult service, a dedicated Leukemia, Lymphoma, Transplant (LLT) elective opportunity, as well as experience as the Medical Admitting Resident (MAR). During the geriatric medicine rotation residents interact with elderly patients in inpatient, outpatient, and home-based settings to gain expertise in the nuances of geriatric medicine. On the medicine consult rotation third-year residents work one-on-one with an attending while interacting with multiple services (surgery, orthopedics, trauma, psychiatry, neurology, etc.) to address pre-operative risk stratification and to manage medical comorbidities and acute medical issues.