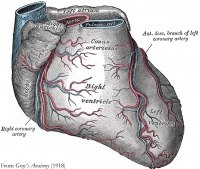
Coronary artery disease (CAD) is caused by plaque buildup in the wall of the arteries that supply blood to the heart; namely, the coronary arteries. Plaque is made up of cholesterol (fat) deposits. For some people, the first sign of CAD is a heart attack.
CAD is the leading cause of death for both men and women in the United States, and every year about 735,000 Americans have a heart attack, according to the Centers for Disease Control and Prevention.
Surgery (coronary artery bypass grafting, or CABG) has long been the gold standard treatment of advanced CAD. Blood is re-directed with arteries and veins to increase blood supply to the heart muscle.
Stents (tube-shaped metal devices) placed by cardiologists are ideal to open up blocked coronary arteries.
Stents provide very good results in patients with less advanced forms of CAD, and are the best emergency treatment for heart attacks. They are placed using a non-surgical procedure known as angioplasty or percutaneous coronary intervention (PCI).
HCR offers patients with multi-vessel CAD the benefits of both bypass surgery and stenting.
Bypass surgery is associated with extended survival, long-lasting relief of chest pain, improved exercise capacity, and minimizing the impact of heart attacks. Patients stay four to seven days in the hospital after bypass surgery, and return to normal activities and/or work in two to three months.
The benefits of PCI are not as long-lasting. However, recovery time after a PCI is short. Patients go home the day after the procedure, and usually can return to normal activities and/or work in seven to ten days.
A promising treatment option for some patients who have blockages in the artery of the front of the heart (left anterior descending artery) and at least one other blockage is a combination of both surgery and stenting, called hybrid coronary revascularization (HCR; revascularization means restoration of blood flow).
First performed in 1996, HCR gained traction toward the end of the first decade of the present century. An increasing number of these procedures are being done now by cardiac surgeons and cardiologists who work together as a team, and who have advanced the technique of doing it.
Here, Jorge M. Balaguer, MD, associate professor of surgery, who is a member of our Cardiothoracic Surgery Division and a leader of the Stony Brook Heart Institute, answers frequently asked questions about HCR in which he has a special interest and expertise. Dr. Balaguer has performed some of the pivotal research showing the safety and effectiveness of HCR.
Q: What is hybrid coronary revascularization, or HCR?
A: HCR is a heart operation that combines coronary bypass surgery with the placement of stents in coronary arteries via a non-surgical procedure. It requires the collaboration of cardiologists and cardiac surgeons to perform it.
The bypass procedure is minimally invasive, using a 2-3 inch incision between the ribs (no bone is divided) on the left side of the chest. This allows the surgeon to perform the bypass graft responsible for extended survival. It has a shorter recovery compared to conventional bypass surgery.
The other blocked arteries are treated with stents that release blood-clot preventing drugs to maximize their effectiveness.
Q: What are the benefits of HCR?
A: HCR offers patients with multi-vessel CAD the benefits of both bypass surgery and stenting. It is minimally invasive, and it does not compromise long-term durability and survival. It integrates the positive features of both CABG and stenting. Currently, it is provided only at a few select medical centers nationwide, including Stony Brook Medicine.
Additionally, benefits of HCR generally are shorter hospital stay, less pain after treatment, less scarring, and faster recovery — benefits that appeal to patients. Indeed, the benefits associated with HCR make treatment of CAD easier to face and easier to undergo.
Q: How is HCR performed? Are surgery and stenting done at the same time?
A: HCR can be performed at one time ("one-stop shop") in an operating room designed for both cardiovascular surgery and PCI stenting, called a hybrid operating room.
Most commonly, HCR is performed in a staged fashion. First, the minimally invasive bypass component is done in a traditional OR and then, after one or two days, the PCI with stent placement is done in a catheterization room.
Q: Must the heart be stopped, as in traditional bypass surgery, to perform HCR?
A: Most of time it is not necessary to stop the heart. The operation is generally performed "off-pump" — without the use of the heart-lung machine to take over the heart's pumping work — and eliminates the need to stop the heart. The surgical component of HCR is minimally invasive. These are the fundamental reasons for the very quick recovery.
Q: How long does the combined HCR procedure usually take?
A: The surgical component takes about three hours. The placement of the stents depends on how many are required. In general, it takes between one and two hours.
Q: How long after HCR can a patient to return to normal activity?
A: Most patients can get back to normal activity in about 3 to 4 weeks. They are discharged home after the procedure in four days or so, and are authorized to drive in seven to ten days.
Q: Has HCR been proven to be as safe and effective as CABG?
A: Yes. Several publications have shown that HCR is a safe procedure. Our own research looked at safety in great detail. It is necessary for the team to be thorough in the selection of patients and for careful planning to be done in the sequence of the surgery and the stenting. Management of some of the medications, especially blood thinners, around the HCR is very important in order to minimize bleeding complications and ensure good functioning of the stents.
Our hybrid ORs make HCR safer and easier in a variety of ways for both patients and physicians.
Q: What are the risks associated with HCR, compared with CABG?
A: Most scientific articles, including our own research and recent publications, show that the risks of HCR are comparable to those associated with conventional CABG. More attention to detail is required in the performance of the surgical component. The sequence of the stenting — before, at the same time, or after the bypass surgery — needs to be individualized to each patient.
Q: What qualifies a patient to be treated with HCR?
A: The anatomy of the coronary artery and the nature of the blockages are the initial determinants. Cardiologist and cardiac surgeon both need to agree that HCR can be performed. Candidacy also needs to be established in view of urgency, chest wall shape, and previous interventions, among other criteria.
Q: Does HCR require a special kind of operating room?
A: No, not necessarily. If the HCR is planned to be done at the same time, the hospital must have a hybrid OR, with capabilities for cardiovascular surgery as well as PCI stenting. Otherwise, the surgery can be done in a traditional cardiac OR, and the stenting a day or two later in a separate catheterization room.
Q: What is the advantage of having HCR done at Stony Brook Medicine?
A: The great collaborative relationship between cardiologists and cardiac surgeons at the Stony Brook Heart Institute makes HCR possible, as the performance of HCR requires teamwork to be successful. This well-established multidisciplinary care model is a major advantage.Another important advantage is the experience we bring to providing HCR, as demonstrated by our pioneering work in HCR and our outstanding track record in bypass surgery, which earned us the highest star rating for outcomes and quality from the Society of Thoracic Surgeons. These attributes are critical components of our HCR program at Stony Brook.
In addition, in the near future we will be performing the surgery part of HCR will the assistance of a surgical robot, which generally minimizes the stress of the bypass surgery. The robotic-assisted approach for HCR involves just three or four incisions less than one-half inch wide.
Currently, our new hybrid ORs, which feature the most up-to-date, technologically sophisticated equipment, enable what I like to call the "one-stop shop" HCR in which both surgery and stenting are done at the same time. This offers patients the advantage of having to undergo a single treatment experience.
Beyond that, our hybrid ORs make HCR safer and easier in a variety of ways for both patients and physicians. They are especially designed to do this.
| "Hybrid coronary revascularization for double-vessel coronary disease is associated with similar short-term outcomes and intermediate-term survival as traditional coronary artery bypass grafting. Hybrid coronary revascularization is associated with lower transfusion requirements and a shorter length of stay than coronary artery bypass grafting.… The excellent short-term and midterm clinical outcomes in these patients support the continued use of a hybrid revascularization strategy for patients with double-vessel coronary disease with appropriate angiographic anatomy." — Journal of Thoracic and Cardiovascular Surgery (2018; see abstract) |