By Tara L. Huston, MD, Assistant Professor of Surgery and Dermatology,
and Leader, Melanoma Management Team
The New England Journal of Medicine just published the results of the Multicenter Selective Lymphadenectomy Trial (MSLT-II). The report includes data from patients who have participated here at Stony Brook Medicine, and is very interesting for a good reason.
MSLT-II is the follow-up to MSLT-I, which provided the basis for utilizing sentinel node biopsy in patients with melanoma).
Lymph nodes are tiny, pea-sized structures throughout the body that work as filters for harmful substances; they contain immune cells that can help fight infection and disease (read more).
The sentinel node biopsy tests the lymph node that drains the melanoma and the skin around it for evidence of cancer. If the sentinel node is unaffected, the cancer is highly unlikely to have spread to surrounding lymph nodes or distant sites in the body.
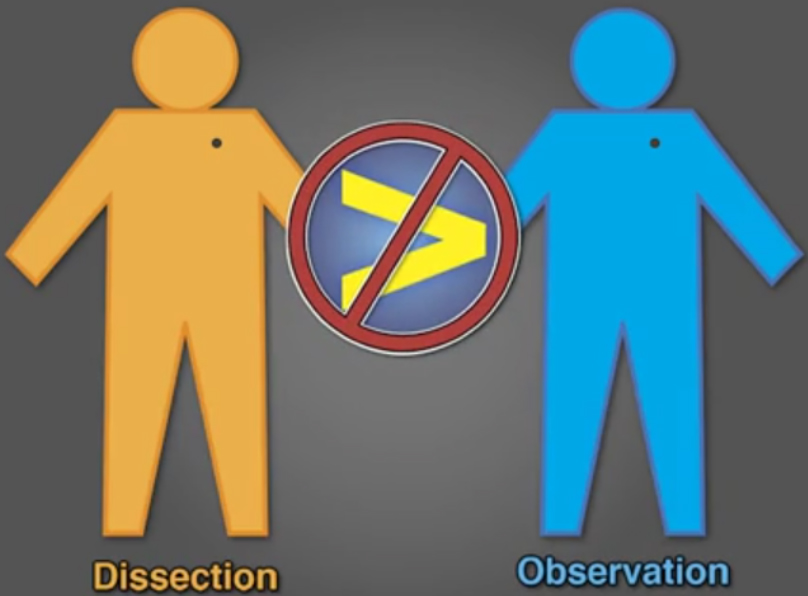
This study, titled "Completion Dissection or Observation for Sentinel-Node Metastasis in Melanoma," sought to answer the question of how to manage metastases (cancer spread) in the sentinel lymph node. Up until now, the treatment was to perform a completion lymph-node dissection; that is, full removal of all lymph nodes in the vicinity of a melanoma skin cancer .
Completion lymph-node dissections risk permanent and debilitating limb swelling. Historically, we know that only about 15% of patients whose melanoma has spread to the sentinel node will have additional disease. That means 85% of patients will not have any further disease, and are subjected to the completion lymph-node dissection.
So, the question we attempted to answer was, Can we safely do follow-up evaluations on these patients, instead of doing invasive surgery on them?
MSLT-II was a prospective, randomized, international, phase 3 (tests safety and efficacy) trial with 1,939 patients. Patients with melanoma in the sentinel node were randomized into immediate completion dissection versus active surveillance with ultrasound of the nodal basin every six months.
Removing all lymph nodes in the vicinity of a melanoma skin cancer was found to
not increase a patient's overall chances for melanoma-specific survival.
| Full lymph-node removal surgery did not increase melanoma-specific survival more than observation with frequent nodal ultrasound. |
This study confirmed that, among patients with melanoma and sentinel-node spread of the cancer, immediate full lymph-node removal surgery increased the rate of regional disease control, and provided prognostic information. However, it did not increase melanoma-specific survival.
The probability of melanoma-specific survival was similar in both the observation and the dissection (removal surgery) groups as far as ten years out from randomization. There was no statistically significant difference. The risk of complications from the lymph-node dissection was nearly 24% in the dissection group versus only 6% in the observation group. The difference in complications was statistically significant.
These findings are important for several reasons. First, they confirm that performing a delayed completion dissection when disease manifests does not result in losing control of the disease. Second, they demonstrate that active surveillance of the nodal basin is a safe and efficient way to identify patients who are most likely to benefit from delayed completion lymph-node dissection.
Lastly and most significantly, they prove no melanoma-specific survival benefit of early completion lymph-node dissection.
Our melanoma program at the Stony Brook Cancer Center continues to offer the most up-to-date treatment options for our patients. This latest research supports our current practice of offering sentinel node biopsy for patients with melanoma deeper than 1 mm (thickness of a dime).
Currently, there are minimal data to support sentinel node biopsy for thin melanomas less than 1 mm deep, although its use may be considered in certain high-risk patients.
| The findings of this study are a game-changer that will protect patients from the debilitating consequences of unnecessary surgery, says Daniel G. Coit, MD, a surgical oncologist at Memorial Sloan Kettering Cancer Center, in his editorial published along with the report. This new study clearly defines the proper role of surgery, Dr. Coit explains. He states, "The findings of the second Multicenter Selective Lymphadenectomy Trial (MSLT-II) … are definitive, unequivocal, and completely consistent both with the published results of retrospective series and with the published results of one previous prospective, randomized, clinical trial." |
Click here to read the study abstract in the New England Journal of Medicine. For appointments with the surgical specialists of the Stony Brook Melanoma Management Team, please call 631-444-4666.