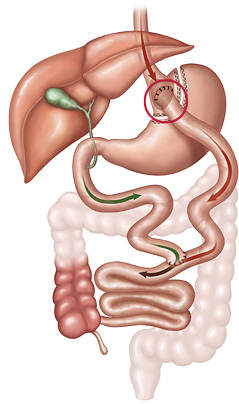
| Roux-en-Y gastric bypass showing the gastrojejunal anastomosis (red circle) where ulcers might occur. |
Bariatric surgery is the most effective treatment for obesity, leading to long-term weight loss, improvements in quality of life, and reduction of obesity-associated medical problems, such as diabetes, sleep apnea, high blood pressure, high cholesterol, venous stasis disease (collection of blood in the lower limbs), and soft-tissue infections.
However, the surgery is associated with possible long-term complications.
Concerns about such complications represent a considerable barrier for eligible patients who consider bariatric surgery. One known long-term post-op complication for the (RYGB) procedure is anastomotic ulceration (AU). Symptoms of ulcer disease include abdominal pain (possibly severe) and nausea, among others.
The RYGB procedure, which currently is the most common bariatric procedure performed in the United States, uses a combination of restriction and malabsorption to reduce calories. During the procedure, the surgeon creates a smaller, egg-sized stomach pouch, using about 5% of the patient's stomach and separating off the rest (see illustration). The surgeon then attaches a section of the small intestine directly to the pouch.
AU is a condition in which ulcers develop where the small intestine is attached to the stomach pouch. Most ulcers of this kind respond to medical therapy, but complicated or complex lesions may require further surgery.
Tobacco-smoking has been implicated in the development of AU, but its role has not been well understood. The questions about it motivated the study just published in JAMA Surgery conducted by faculty in our Bariatric, Foregut, and Advanced Gastrointestinal Surgery Division.
A significant long-term risk of anastomotic ulceration after Roux-en-Y gastric bypass is associated with passage of time and history of tobacco use.
The title of the study is "Association of Long-term Anastomotic Ulceration after Roux-en-Y Gastric Bypass with Tobacco Smoking" (see preview). The first author of the study is Konstantinos Spaniolas, MD, associate professor of surgery and associate director of the Stony Brook Bariatric and Metabolic Weight Loss Center.
The aim of this study, according to the authors, was to describe the epidemiology of AU after RYGB and measure the association of tobacco smoking with long-term AU incidence.
The Statewide Planning and Research Cooperative System database of the Department of Health of New York State was used to identify 35,075 adult patients who underwent laparoscopic or open RYGB for obesity in the state of New York in 2005 through 2010.
The study found that 17.8% of patients with a history of tobacco use at the time of RYGB surgery developed AU within eight years. These findings emphasize the need for proper patient and bariatric procedure selection.
The authors conclude: "The findings of this study underline that the incidence of AU after RYGB is more common than previously reported and that it progressively increases over time.
"Despite the limitations of the retrospective design, the lack of bariatric-specific granular data, and the possibility of missing patients with AU who were diagnosed and managed exclusively outside the hospital setting, the long-term effect of tobacco use on this complication is profound.
"Such information can potentially aid in procedure selection at the time of initial bariatric surgery or guide patient selection for targeted AU preventive and surveillance strategies."
Dr. Spaniolas told Reuters Health, "The findings can be used to tailor procedure selection for patients with exposure to tobacco, potentially steering them away from gastric bypass and towards other bariatric procedures, or extending ulcer prophylaxis measures lifelong for such individuals who undergo gastric bypass.
"Additionally, [our study] reinforces the possible value of long-term bariatric follow up, specifically in an attempt to identify and aggressively treat (these ulcerations) early in their stage of development."
Studies like this conducted by our faculty demonstrate that not only do they take care of patients, they make surgery better through research. This is what sets us apart.
| Stony Brook Medicine is shaping the future of bariatric surgery on multiple fronts. Reflecting the vision and leadership of its founder and director, Aurora Pryor, MD, and associate director, Konstantinos Spaniolas, MD, the Bariatric and Metabolic Weight Loss Center has become a leader nationally and internationally through advanced clinical care, research, advocacy, and mentorship of the next generation of surgeons (read more). |

