
The medical innovations and breakthroughs made by Stony Brook’s basic science and clinical researchers have been both life-saving and transformative. Their cutting-edge research has led to the development of radical new treatments, diagnostic tools and surgical techniques, significantly improving patient outcomes and quality of life worldwide. Throughout Stony Brook’s illustrious history, numerous innovations have emerged, including these ten breakthroughs that have revolutionized the field of medicine.
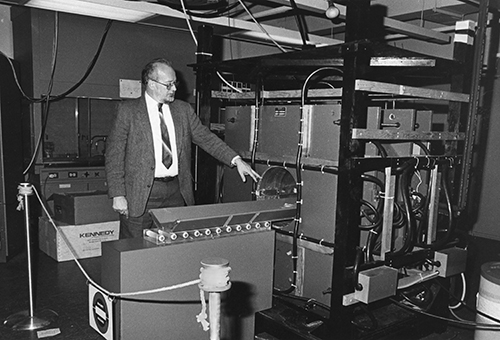
Development of Magnetic Resonance Imaging (MRI); creation of the first MRI image of a living organism
In 1973, two years after jotting notes from a “Eureka” moment he had inside a Pennsylvania Big Boy, Stony Brook chemistry professor Paul C. Lauterbur published a paper regarding a new technique in which he could introduce gradients in the magnetic field utilized for nuclear magnetic resonance (NMR) and analyze the spatial data collected to produce multi-dimensional images of organs and soft tissues. Creating the first such image of a living organism—a baby clam his daughter found near Setauket Harbor—within the Chemistry building at Stony Brook University, Dr. Lauterbur’s non-invasive technique and further research led to the development of one of the most important medical innovations in the twentieth century: magnetic resonance imaging, more widely known as the MRI. Today, US medical professionals perform an average of 30 million MRI scans every year. For his technological breakthrough, Dr. Lauterbur was awarded the Nobel Prize in Physiology or Medicine in 2003.
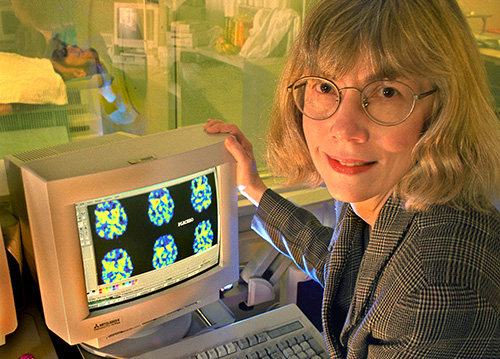 PHOTO: Courtesy of Brookhaven National Laboratory.
PHOTO: Courtesy of Brookhaven National Laboratory.
Advancements in PET imaging technology
Beyond its pioneering role in MRI technology, Stony Brook has been equally vital to the evolution of positron emission tomography (PET) imaging. In 1976, Dr. Joanna S. Fowler, an Emeritus Adjunct Professor from Stony Brook's Department of Chemistry, was Director of Radiotracer Chemistry at the US Department of Energy's Brookhaven National Laboratory (BNL) when she and her team successfully synthesized 18F-fluorodeoxyglucose (FDG), a crucial radiotracer for PET imaging. Today, FDG-PET imaging is a staple in medical facilities worldwide, aiding in brain research and cancer diagnosis. Dr. Fowler's groundbreaking work earned her the prestigious National Medal of Science at the White House in October 2009, recognizing her significant contributions to neuroscience and disease research, particularly in addiction studies.
Determining the cause of Lyme disease
Lyme disease, which stems from borrelia bacteria transmitted by ticks, is one of the most prevalent tick-borne illnesses on Long Island. In 1982, Dr. Jorge Benach, Distinguished Professor at Stony Brook's School of Medicine, collaborated with National Institutes of Health (NIH) scientists to identify and isolate Borrelia burgdorferi, the causative agent. Published in prestigious journals like Science and The New England Journal of Medicine, Dr. Benach’s work cemented Stony Brook University Hospital's standing as a leading research center. Dr. Benach, who also served as Director of Stony Brook's Center for Infectious Diseases, was honored as a 2010 Fellow of the American Association for the Advancement of Science.
In August 2023, Stony Brook Southampton Hospital launched its Regional Tick-Borne Disease Center, the Northeast's first dedicated tick clinic. Here, infectious disease specialists diagnose and treat patients for tick bites and associated illnesses, reinforcing the region's efforts against tick-borne diseases.

Uncovering the link between emphysema and smoking
Throughout the 1970s and 1980s, Aaron Janoff, PhD, a Professor of Pathology at Stony Brook, published multiple articles that revealed commonalities between emphysema and smoking, building the case that the two were closely linked. His work, including a notable July 1988 article in Chest, the official publication of the American College of Chest Physicians (“Elevated histamine and tryptase levels in smokers' bronchoalveolar lavage fluid. Do lung mast cells contribute to smokers' emphysema?”), provided research findings that highlighted the correlation and firmly supported the conclusion that smoking could increase histamine activity in the lungs, exacerbating inflammation and allergic reactions. Dr. Janoff’s crucial contributions in understanding the health impacts of smoking earned him accolades such as the NIH MERIT award and the American Thoracic Society Presidential Citation in 1987, as well as prestigious awards like the Alton Ochsner Award Relating Smoking and Health.
Synthesizing poliovirus
In 1991, Dr. Eckard Wimmer, a Distinguished Professor and former Chair of the Department of Microbiology & Immunology at the Renaissance School of Medicine, achieved a significant milestone by publishing the first cell-free synthesis of a virus (poliovirus), revolutionizing viral replication studies. In 2002, he and his team followed this accomplishment with the first chemical-biochemical test-tube synthesis of a virus (again, poliovirus), without a natural template. Despite post-9/11 concerns about potential misuse, Dr. Wimmer's work catalyzed extensive research in virology and cell biology, pushing the boundaries of virus structure and function exploration. His contributions earned global recognition and accolades, including being named a Fellow of both the National Academy of Sciences and the American Association for the Advancement of Science. In 2012, he received the esteemed Robert Koch Gold Medal, an international scientific honor presented by the Robert Koch Foundation under the patronage of the German Minister of Health.

Pioneering 3-D virtual colonoscopy technology
In the early 1990s, Arie E. Kaufman, PhD, Distinguished Professor and Chair of Stony Brook’s Department of Computer Science, along with Jerome Zhengrong Liang, PhD, Co-Director of Radiology Research, began work on what evolved into a revolutionary medical imaging breakthrough: 3-D virtual colonoscopy (VC). Their FDA-approved application-driven innovation revolutionized colon cancer screenings, offering an accurate, faster and less invasive alternative to traditional colonoscopies. Dr. Liang's contributions to medical image reconstruction and virtual colonoscopy earned him the Institute of Electrical and Electronics Engineers (IEEE) Fellow Award in 2007. In April 2018, Dr. Kaufman was inducted as a Fellow of the National Academy of Inventors (NAI) in recognition of his research and innovations in 3-D VC technology, which has significantly improved patient comfort and procedure efficiency.

A preventive life-saver in ReoPro®
Barry S. Coller, MD, a former Distinguished Service Professor of Medicine and Pathology, and his landmark research on the rare platelet disorder Glanzmann thrombasthenia at Stony Brook’s School of Medicine, resulted in the development of the drug Abciximab. In 1994, in collaboration with scientists at biopharmaceutical company Centocor, Dr. Coller’s Abciximab became the first drug developed from SUNY technology to be approved by the US Food and Drug Administration for marketing in the United States. Marketed as ReoPro® the following year, the groundbreaking medication aided millions of patients in the prevention of heart attacks after angioplasty and stent procedures.

Changing the future of antiviral drug development
At the onset of the AIDS pandemic, Carol Carter, PhD, Distinguished Professor of Microbiology and Immunology, Adjunct Professor of Physiology and Biophysics, and an early pioneer in the HIV research field, advanced understanding of the viral-encoded protease and purified the viral capsid protein for structural and biochemical studies. In 2001, Dr. Carter’s groundbreaking research, published in the Proceedings of the National Academy of Sciences (PNAS), identified an interaction between HIV and a host protein (Tsg101) that is essential for the assembly and budding of HIV viral particles from infected cells. Her findings opened a new field of research on host factors in microbial pathogenesis and suggested the possibility of targeting host proteins for developing antimicrobial therapeutics, with implications beyond HIV. As a result of her pioneering work, Dr. Carter was elected to the National Academy of Sciences in 2024.
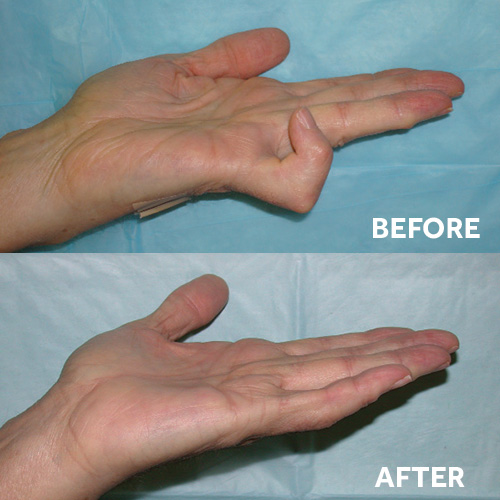
A non-surgical breakthrough with Xiaflex®
In February 2010, the US Food and Drug Administration approved a novel medication for Dupuytren’s contracture, a debilitating hand disorder caused by the progressive buildup of collagen, resulting in finger deformities and limited mobility. Developed by Marie A. Badalamente, PhD, and Lawrence C. Hurst, MD, Department of Orthopaedics, the drug, called Xiaflex®, became the first FDA-approved non-surgical treatment for Dupuytren’s contracture. Previous FDA-approved clinical trials demonstrated significant improvement in patient outcomes with this injectable form of the enzyme collagenase. In December 2013, Xiaflex® also became the first FDA-approved treatment for Peyronie’s disease, a painful penile curvature resulting from plaque accumulation beneath the skin of the penis.
Innovating a new ultrasound method that speeds the healing of bone fractures
In 2012, Yi-Xian Qin, PhD, Professor, Department of Biomedical Engineering, and Director of the Orthopaedic Bioengineering Research Laboratory at Stony Brook University, and his research team demonstrated how medium-intensity focused ultrasound can bolster the mobility of osteoblasts, the cells responsible for bone formation, and activate calcium release, the process that promotes growth. Dr. Qin and his team detailed their method, which has contributed heavily toward developing non-pharmacologic treatments of osteoporosis, fractures and other conditions involving bone loss, in the PLoS (Public Library of Science) One article “Mechanobiological Modulation of Cytoskeleton and Calcium Influx in Osteoblastic Cells by Short-Term Focused Acoustic Radiation Force.”