Patients More Likely to Receive Repair Than Replacement from Most Experienced Surgeons
The mitral valve is the most complex of the heart's four valves, and is the one most commonly associated with disease. It is located between the left heart chambers (left atrium and left ventricle). In mitral valve disease, it doesn't work properly.
There are three main conditions that affect the valve: obstruction (stenosis), leakage (regurgitation), and bulging backward during valve closure (prolapse).
Prolapse is the most common, occurring in up to 5% of the population, whereas stenosis is the least common, accounting for less than 1% of cardiac diagnoses in the United States, although it is more frequently seen in developing nations.
A faulty mitral valve that is not causing symptoms — cough, shortness of breath, swollen feet or legs, chest pain, fatigue, lightheadedness — may not need any treatment. Mild symptoms may be treated with medicine. With more severe symptoms, surgery may be required.
Most mitral valve surgeries have a low rate of complications, according to the Society of Thoracic Surgeons. However, potential complications include bleeding, infection, blood clots, irregular heart rhythm, or heart attack.
The contribution of surgeon-specific factors in the outcomes of mitral valve surgery is poorly defined. Thus, Joanna Chikwe, MD, our chief of cardiothoracic surgery and co-director of the Stony Brook Heart Institute, and her colleagues at Mount Sinai Heart, conducted a study to evaluate the influence of surgeon case volume.
The study, of which Dr. Chikwe is lead author, was published last month in the Journal of the American College of Cardiology, titled "Relation of Mitral Valve Surgery Volume to Repair Rate, Durability, and Survival." It was featured on TCTMD. The findings were simultaneously presented at the American Association for Thoracic Surgery Centennial meeting in Boston.
"Look at not just the number of mitral valve operations in the surgeons,
but what his or her repair rates actually are."
"We were able to show that durability of repair was actually about three times as good in patients operated on by surgeons doing more than 25 mitral valve operations per year," Dr. Chikwe says.
"And that translates into even better survival at one year. More patients were likely to be alive at one year if they had their mitral valve repair done by a high-volume surgeon."
Dr. Chikwe adds that volume is used as a surrogate for expertise, but it doesn't tell the full story: "On its own, the number [of mitral valve surgeries] doesn't necessarily predict that you'll have a good repair.
"I think what we're really trying to encourage with referring physicians and patients is to look at not just the number of mitral valve operations in the surgeons, but what his or her repair rates actually are."
Guidelines in the U.S. and Europe recommend valve repair instead of valve replacement when possible, according to the researchers, although they mentioned mitral valve replacement remains common in patients with degenerative valve disease.
This study included 5,475 adults who underwent primary mitral valve operations in New York between 2002 and 2013 and were part of the Statewide Planning and Research Cooperative System, an all-payer, administrative database.
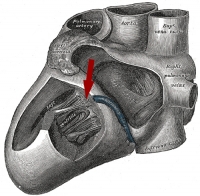
| Illustration of heart from Gray's Anatomy showing location of bicuspid valve, another name for mitral valve (click on image to enlarge). |
The researchers reviewed all of the patient data before the operation and followed up patients for at least 12 months after the procedure. They also identified 313 surgeons from 41 institutions who met their eligibility criteria.
Patients who saw surgeons with less than 25 operations in a year were significantly more likely to present as urgent admissions and were more likely to have congestive heart failure, chronic kidney disease, or chronic airway disease, compared with patients who were operated on by surgeons with higher total annual surgeon volumes.
After the researchers adjusted for multiple variables, they found that the total annual surgeon volume was independently associated with the probability of mitral valve repair. They mentioned the probability of repair increased by 13% for every 10-case increment in total annual surgeon volume.
Patients who were operated on by surgeons with a total annual surgeon volume of more than 50 operations were more than three times as likely to undergo mitral valve repair compared with those who were operated on by surgeons with an annual surgeon volume of 10 or fewer operations.
They also found a significant association between low surgeon volume and increased risk of mitral valve reoperation within 12 months of follow-up after mitral valve repair.
The cumulative incidence of reoperation at 12 months was 1.3% for patients operated on by a surgeon with a total annual surgeon volume of 25 or more operations, compared with 3.6% for patients operated on by a surgeon with total annual surgeon volume of less than 25 operations.
Although mitral repair was significantly associated with better survival compared with mitral replacement, the total annual surgeon volume remained a significant independent predictor among patients undergoing mitral replacement, according to Dr. Chikwe and her colleagues.
| "This study adds further clarity to the American Heart Association and American College of Cardiology guidelines, which already recognize that patients with degenerative mitral valve disease should be referred to experienced mitral surgeons whenever feasible," says senior study author David H. Adams, MD, who is cardiac surgeon-in-chief at Mount Sinai. "Our study found for the first time that individual surgeon volume was directly linked to freedom from reoperation and survival after one year in patients operated on for degenerative mitral valve disease." |
See Dr. Chikwe's study in the Journal of the American College of Cardiology; see video (2:16 min) in which she explains it. For consultations with her and our other experienced mitral surgeons, please call 631-444-1820.

