Our goal is to provide internal medicine residents with a strong foundation in ambulatory medicine since the majority of healthcare in the United States occurs in the outpatient setting. In the 4+1 block system, residents will have 1 week of continuity clinic every 5th week.
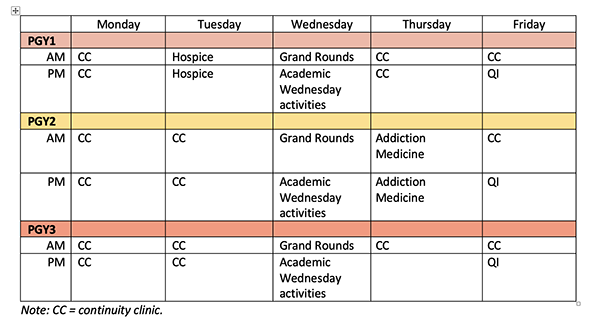
Upon matching to our program, residents are assigned to either the Stony Brook Primary Care Center (PCC) or the Northport Veterans Affairs Primary Care Clinic for their continuity clinic. During this outpatient week, residents provide primary care to a panel of patients at their assigned clinics and will spend part of the year working in subspecialty clinics to broaden their outpatient skills. Below is an example of a typical clinic week during each PGY year:
Ambulatory Didactics

During their ambulatory week, residents participate in case-based didactic workshops that focus on a variety of outpatient topics. To supplement these education workshops, residents also have access to multiple online outpatient education curricula, such as the: Physician Education & Assessment Center- Internal Medicine Curriculum, American College of Physician’s Caring with Compassion, and the Center for Advanced Palliative Care training modules.
Quality Improvement Projects
During their clinic experience, all residents learn how to conduct a quality improvement project and will work in teams to complete an outpatient QI project together. Examples of resident-led QI projects include:
Current Projects at the Stony Brook Primary Care Center
- Improving Colon Cancer and Cervical Cancer Screening
Residents are creating workflows in clinic that engage all members of the interdisciplinary team to help improve screening rates
Prior Projects at the Stony Brook Primary Care Center
- Safe opiate prescribing for non-cancer related chronic pain
Residents developed and implemented workflows to meet the standards of safe opiate prescribing. Our clinic has been identified as a QI Champion for the American College of Physicians and was highlighted as one of the best education research projects in 2018 by the Alliance of Academic Internal Medicine (AAIM). This project was also published in Pain Medicine:
o Wong R, Carroll W, Muttreja A, Garcia V, Taub E, Fernan A. Improving Opioid Management and Resource Utilization in an Internal Medicine Residency Clinic: A Before-After Study over Two Plan-Do-Study-Act Cycles. Pain Med. 2019;20(10):1919-1924. doi:10.1093/pm/pny239
- Improving chronic care management for patients with diabetes
Residents obtained point of care A1c testing for our clinic and implemented diabetic foot care examination kits in each clinic room. - Improving weight loss management for patients with obesity
Residents created tailored patient education for the EMR and improved referral workflows to Stony Brook’s Weight Management Center. - Improving patient portal access
Residents created education materials and workflows to increase patient participation in our EMR’s patient portal.

Current Projects at the Northport VA Primary Care Clinic:
- Ensuring proper Eliquis dosing in veterans
- Increasing face time between physicians and patients by instituting dedicated triage time for nursing
- Improving vaccination rates in patients with cirrhosis
- Promoting multi-modal smoking cessation strategies for veterans
- Implementing a population management strategy to improve diabetes metrics
- Assessing veterans with a listed penicillin allergy and evaluating the potential to de-label
- Utilizing opioid education to increase Narcan prescriptions to veterans with chronic pain on opioids
Prior Projects at the Northport VA Primary Care Clinic:
- Improving Coordination of Care of Heart Failure Patients in the Outpatient Setting
- Utilizing and Increasing access to telehealth
- Coordinating with prosthetics dept
- Identifying patients for PACT PharmD CHF Clinic
- Goal to implement a CHF Menu into EMR
- Improving Timely and Appropriate Medication refills/renewals in PC Clinic
- Increasing the number of patients with lab work prior to presenting to PCP Appointment
- Improving Non-VA Medication Reconciliation
- Increasing Goals of Care Discussion in an Outpatient Setting
- Implementation of a lung cancer screening database
- Increasing HIV and HCV Screening
- Improving TDap/TD Immunization
- Resident-driven population management to improve primary care statin and blood pressure measures
- Promoting safe gun storage among veterans to prevent and reduce fun-related suicide and accidents
Stony Brook Primary Care Center

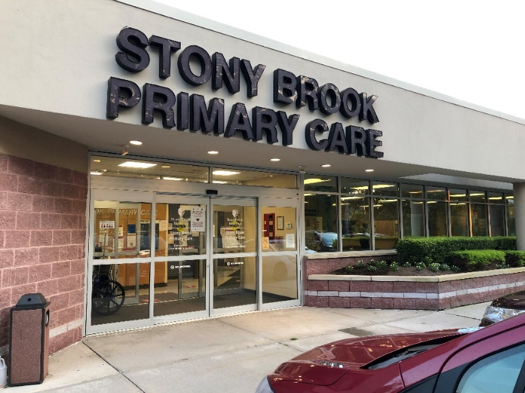
The Stony Brook Primary Care Center (PCC, aka Tech Park Clinic) is located at 205 N. Belle Mead Road, East Setauket, NY and is the primary outpatient practice for the Division of General, Geriatric and Hospital Medicine.. The PCC is a certified Level 3 Patient Center Medical Home that provides primary care to a wide variety of patients in Eastern Long Island. Residents who are assigned to the PCC for their continuity clinic learn how to provide comprehensive preventive and chronic care management via in-office and telehealth visits. Residents also have the unique opportunity to work closely with the clinic’s Integrated Behavioral Health Team, which includes Stony Brook psychiatrists and psychologists to provide mental health services for PCC patients.
To learn more about the General Internal Medicine faculty, please visit: https://renaissance.stonybrookmedicine.edu/medicine/geriatrics/faculty
Northport Veterans Affairs Primary Care Clinic

The Northport VA Primary Care Clinic is located at 79 Middleville Road, Northport, NY 11768 and serves a wide age range of veterans, some of whom are still on active duty. As part of the largest national healthcare network, the Clinic is conveniently located in the same building as the Laboratory, Pharmacy, Radiology, Emergency Department, Subspecialty Clinics, and Inpatient Hospital/Intensive Care Unit, which provides for a convenient and seamless transition for our deserving veterans. Each clinic is a PACT (Patient Aligned Care Team) with a range of interdisciplinary team members (Social Work, Primary Care Mental Health, PharmD, etc.) to ensure our veterans receive the best possible care. As a pioneer in telemedicine, the VA is also able to provide veterans with an iPad to ensure they continue to receive comprehensive primary care throughout the pandemic and is able to monitor veterans remotely on a daily basis if diagnosed with COVID-19 and self-quarantining at home. As such, residents are adept at providing care via in-person visits as well as telemedicine visits, ensuring they are well trained for life after residency. A dedicated VA Chief helps to oversee the resident-run QI curriculum associated with the Office of Academic Affairs and the National Center for Patient Safety, targeting local issues with the aim to improve the care our veterans receive and their overall experience at the VA.