Patient Safety Education
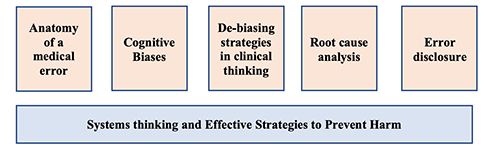
The Patient Safety curriculum prepares our residents to apply fundamental patient safety concepts into their current and future clinical care. The curriculum is focused on harm prevention and strategies used to mitigate medical errors. Residents work in small groups to learn key concepts in patient safety using mock mortality cases and video scenarios. Topics include cognitive biases, adverse events, sentinel events, root cause analysis, and failure mode effect analysis. Our safety program highlights the Just Culture model - one that supports the discussion of adverse events and unexpected outcomes. Residents engage in sharing their own clinical experiences and work together to create de-biasing strategies to prevent errors. In order to ensure that our residents are further prepared to tackle all aspects of patient safety, a dedicated educational activity on error disclosure is part of the curriculum. This session focuses on key skills that our resident will need to conduct bedside disclosure of unexpected outcomes in their future clinical practice.
Core Topics in Patient Safety Education
The patient safety curriculum does not end with classroom workshops and discussion. The Stony Brook Internal Medicine Residency integrates patient safety into multiple aspects of residency training.
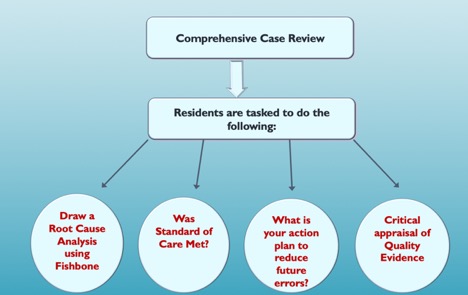
Morbidity, Mortality and Improvement Conference (MM&I) – is an expansion of our efforts to promote harm prevention and strategies to promote safe patient care. We take pride in promoting the just culture and maintaining collegial relationships with other departments and disciplines during our monthly MM&I conferences. Our multidisciplinary MM&I is focused on a systems approach – the objective of the investigation and analysis is the prevention of future adverse events. We implemented our “Learning from Errors” curriculum that refocuses the content and transforms M&M into a platform for teaching patient safety principles and emphasizing error reduction strategies. Cases are presented in a workshop-style format followed by small group activity in which trainees are assigned specific safety tasks based on level of training: 1) systematic analysis of an error, 2) conduct root cause analysis, 3) resident peer review and creation of an action plan.
URL for Stony Brook Internal Medicine M,M&I curriculum: https://www.mededportal.org/doi/full/10.15766/mep_2374-8265.10462
Event Reporting Workshop
Our residents are actively engaged in identifying and reporting safety events that occur during routine patient care. We implemented a structured educational workshop on the process of event reporting and its impact on patient care. We partnered with our Graduate Medical Education department to provide feedback to our residents on outcomes associated with event report entries. The Internal Medicine residents have reported some of the highest numbers of events over the past few years.
Kevin Zarrabi , Kelly Cummings , Nicole Lum , Erin Taub & Nirvani Goolsarran (2020) A resident-led initiative to improve patient safety event reporting in an internal medicine residency program, Journal of Community Hospital Internal Medicine Perspectives, 10:2, 111-116, DOI: 10.1080/20009666.2020.1740507
Quality Improvement Education (QI)
The Quality Improvement (QI) curriculum integrates didactics, small group discussion and project-based learning. The curriculum provides an overview of concepts and methodologies for process improvement. Lectures cover a variety of topics, from basic concepts in quality to newer subjects such as the role of electronic health records and QI research. The curriculum is designed to integrate residents into the healthcare system and provides hands-on experiences in implementing and analyzing quality processes and prepare trainees to be able to implement continuous quality improvement in their future practices. The residents work on group QI projects in their ambulatory clinics that are aligned with the aims of the Patient Centered Medical Home. Projects are in alignment with our quality metrics and desired outcomes in the ambulatory setting.
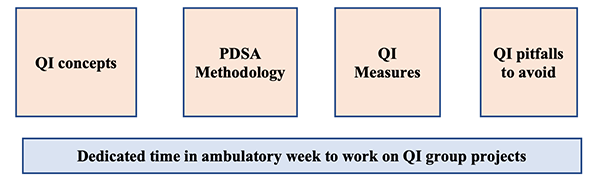
During their clinic experience, all residents learn how to conduct a quality improvement project and will work in teams to complete an outpatient QI project together. Examples of resident-led QI projects include:
Current Projects at the Stony Brook Primary Care Center
- Reducing the Cost of Medications for Patients
Residents are aiming to Improve the utilization of a Real-Time Prescription Drug Benefits (RTPB) Tool in our electronic health record, which displays accurate prescription drug benefit information at the point of prescribing, among the providers at Stony Brooks Primary Care Center
- Improving Preventative Healthcare
Residents are creating workflows to improve the rate of annual visits, including Annual Medicare Wellness Visits, completed in the resident clinic
Prior Projects at the Stony Brook Primary Care Center
- Safe opiate prescribing for non-cancer related chronic pain-
Residents developed and implemented workflows to meet the standards of safe opiate prescribing. Our clinic has been identified as a QI Champion for the American College of Physicians and was highlighted as one of the best education research projects in 2018 by the Alliance of Academic Internal Medicine (AAIM). This project was also published in Pain Medicine:- Wong R, Carroll W, Muttreja A, Garcia V, Taub E, Fernan A. Improving Opioid Management and Resource Utilization in an Internal Medicine Residency Clinic: A Before-After Study over Two Plan-Do-Study-Act Cycles. Pain Med. 2019;20(10):1919-1924. doi:10.1093/pm/pny239
- Wong R, Carroll W, Muttreja A, Garcia V, Taub E, Fernan A. Improving Opioid Management and Resource Utilization in an Internal Medicine Residency Clinic: A Before-After Study over Two Plan-Do-Study-Act Cycles. Pain Med. 2019;20(10):1919-1924. doi:10.1093/pm/pny239
- Improving chronic care management for patients with diabetes
Residents obtained point of care A1c testing for our clinic and implemented diabetic foot care examination kits in each clinic room. - Improving weight loss management for patients with obesity
Residents created tailored patient education for the EMR and improved referral workflows to Stony Brook’s Weight Management Center. - Improving patient portal access
Residents created education materials and workflows to increase patient participation in our EMR’s patient portal.
VA Projects
- Improving Coordination of Care of Heart Failure Patients in the Outpatient Setting
- Utilizing and Increasing access to telehealth
- Coordinating with prosthetics dept
- Identifying patients for PACT PharmD CHF Clinic
- Goal to implement a CHF Menu into EMR
- Improving Timely and Appropriate Medication refills/renewals in PC Clinic
- Increasing the number of patients with lab work prior to presenting to PCP Appointment
- Improving Non-VA Medication Reconciliation
- Increasing Goals of Care Discussion in an Outpatient Setting
- Implementation of a lung cancer screening database
- Increasing HIV and HCV Screening
- Improving TDap/TD Immunization