The Division of Pediatric Anesthesiology aims to provide outstanding family-centered centered care. We have a mandate to develop a collaborative culture of excellence in pediatric perioperative medicine with an emphasis on education, clinical research, and the projection of our unique skill set throughout the hospital system.
Our group has expertise in all techniques of anesthesia that may benefit neonates, infants, and children of all ages. Team members have particular interest and skills in the provision of regional analgesia for pain relief, the application of enhanced recovery pathways that can minimize the impact of surgery, and efforts to both measure and improve the quality of recovery following surgery.
Team members fill key leadership positons at the university and in several national and international collaborative efforts. We gladly bring this cutting-edge experience to the community for the benefit of our patients.
Our group has expertise in all techniques of anesthesia that may benefit neonates, infants, and children of all ages. Team members have particular interest and skills in the provision of regional analgesia for pain relief, the application of enhanced recovery pathways that can minimize the impact of surgery, and efforts to both measure and improve the quality of recovery following surgery.
Team members fill key leadership positons at the university and in several national and international collaborative efforts. We gladly bring this cutting-edge experience to the community for the benefit of our patients.
Division Members
 Chief of Pediatric Anesthesia |
|
- Ehab Al-Bizri, MD.
- Zvi C. Jacob, MD, FAAP
- Ronald C. Jasiewicz, DO, MBA, FAAP
- Paul Kozlowski, MD
- Ashley Mathew, MD
- Vahé S. Tateosian, MD.
Residency Training
- During the first clinical year in anesthesia training (CA-1), residents are introduced to the subspecialty of pediatric anesthesia. This introduction includes providing care for pediatric surgery cases, as well as participating in a didactic lecture series provided by the pediatric anesthesia faculty, which introduces the fundamental principles of pediatric anesthesia.
- The CA-2 resident rotation requires a minimum of two months. The first month takes place at at our ambulatory surgery center. This is a stand-alone surgical center located next to the main hospital. This rotation provides great practical exposure to routine pediatric anesthesia care in the ambulatory setting. Most of the patients are greater than six months of age and are otherwise healthy. The residents are under a “one-to-one” ratio coverage by our team members, which allows close supervision and teaching. The second month of the rotation takes place at the main hospital. This part is designed to let the trainee gain experience in providing anesthesia to sicker patients and working with various surgical subspecialties. Part of the time the trainee will be working at the out-of-OR locations (radiology, GI, etc).
- CA-3 residents undergo one month of advanced pediatrics rotation. This rotation allows the residents to further grow their skills and knowledge in treating the most challenging patients. The prime goal is to lead and encourage our residents to develop the skills and knowledge necessary to become a consultant anesthesiologist.
Residents will also be encouraged to participate in research activities. Members of the pediatric anesthesia division have a number of publications in peer-reviewed journals, presentations at regional and national conferences, as well as published book chapters. This provides the opportunity for residents with interest in pediatric anesthesia to become active participants in research and professional writing.
The pediatric anesthesia division has a dedicated lecture series as part of weekly residents’ academic days and includes keyword lecture series, problem based learning discussions, and faculty lectures.
Division members also participate in and organize medical missions to third world countries. These missions are designed to bring state of the art anesthesia care and education to underserved areas of the world. This outreach effort consistently includes residents who always gain valuable learning and clinical experiences. Recent missions include trips to the Philippines in 2011 and 2013.
The pediatric anesthesia division has a dedicated lecture series as part of weekly residents’ academic days and includes keyword lecture series, problem based learning discussions, and faculty lectures.
Division members also participate in and organize medical missions to third world countries. These missions are designed to bring state of the art anesthesia care and education to underserved areas of the world. This outreach effort consistently includes residents who always gain valuable learning and clinical experiences. Recent missions include trips to the Philippines in 2011 and 2013.
Recent Division Activity
 |
Recent Publications
Resident authors denoted by bold type
- Rove KO, Strine AC, Wilcox DT, Vricella GJ, Welch TP, VanderBrink B, Chu DI, Chaudhry R, Zee RS, Brockel MA; PURSUE Study group (Moore RP). Design and development of the Pediatric Urology Recovery After Surgery Endeavor (PURSUE) multicentre pilot and exploratory study. BMJ Open. 2020 Nov 23;10(11):e039035. doi: 10.1136/bmjopen-2020-039035.
- Doan LV, Padjen K, Ok D, Gover A, Rashid J, Osmani B, Avraham S, Wang J, Kendale S. Relation between preoperative benzodiazepines and opioids on outcomes after total joint arthroplasty. Sci Rep. 2021 May 18;11(1):10528.
- Naftalovich R, Iskander AJ, Eloy JD, Tateosian VS, Naftalovich D. The Case for Bougie Consideration in Every Intubation. Air Med J. 2021 Jul-Aug;40(4):194.
- Moore RP, Burjek NE, Brockel MA, Strine AC, Acks A, Boxley PJ, Chidambaran V, Vricella GJ, Chu DI, Sankaran-Raval M, Zee RS, Cladis FP, Chaudhry R, O'Reilly-Shah VN, Ahn JJ, Rove KO; PURSUE Study Group. Evaluating the role for regional analgesia in children with spina bifida: a retrospective observational study comparing the efficacy of regional versus systemic analgesia protocols following major urological surgery. Reg Anesth Pain Med. 2023 Jan;48(1):29-36.
- Hafeman M, Greenspan S, Rakhamimova E, Jin Z, Moore RP, Al-Bizri E. Caudal block vs. transversus abdominis plane block for pediatric surgery: a systematic review and meta-analysis. Front Pediatr. 2023 May 30.
- Tsivitis A, Wang A, Murphy J, Khan A, Jin Z, Moore R, Tateosian V, Bergese S. Anesthesia, the developing brain, and dexmedetomidine for neuroprotection. Frontiers Neurol. 2023 Jun 7.
- Burjek NE, Hafeman M, Guthrie D, Desai A, Jin Z, Brockel M, Moore R. Perioperative use of gabapentinoids in pediatric patients. APS 2023:1, 21.
- Zhang DA, Brenn B, Cho R, Samdani A; Shriners Spine Study Group (Moore RP); Poon SC. Effect of gabapentin on length of stay, opioid use, and pain scores in posterior spinal fusion for adolescent idiopathic scoliosis: a retrospective review across a multi-hospital system. BMC Anesthesiol 2023 Jan 7;23(1):10.
- Tsivitis A, Kozlowski P, Corrado T, Chesler D, Moore R, Al-Bizri E. Traumatic carotid artery injury caused by a metal sipping straw in a pediatric patient: Anesthetic management and considerations. Trauma Case Rep. 2023 Oct 20;48:100965.
- Ozturk B, Koundal S, Al-Bizri E, Chen X, Gursky ZH, Dai F, Lim AS, Heerdt P, Kipnis J, Tannenbaum A, Lee H, Benveniste H. Continuous positive airway pressure (CPAP) increases CSF flow and glymphatic transport. JCI Insight. 2023 May 9.
- Shafai A, Tateosian V. The Path Toward a Sustainable Global Health Partnership. ASA Monitor. 2023 Apr;87: 35.
- Wang A, Tsivitis A, Ma S, Jin Z, Al-Bizri E, Moore R. The safety and efficacy of sugammadex for reversing neuromuscular blockade in younger children and infants. Expert Opin Drug Saf. 2024 Jun 28.
- Desai A, Razak A, Ghaly L, Bennici L, Moore R. Opioid-Obviating Analgesia for Adolescent Multilevel Spinal Fusion Surgery: A Problem-Based Learning Discussion. A A Pract. 2024 Jul 11;18(7):e01823.
- Elias M, Tateosian VS, Richman DC. What's New in Preoperative Cardiac Testing. Anesthesiol Clin. 2024 Mar;42(1):9-25.
- Tsivitis A, Hafeman M, Tateosian VS, Weinhold A. Pediatric Anesthesia: Giggle Gas, Time Travel, and Working with the Best Population. ASA Monitor. 2024 Sep;88: 33.
- Gilbertson LE, Muhly WT, Montana MC, Chidambaran V, DiCindio S, Sadacharam K, Wilder RT, Whyte SD, Hifko A, Sponseller PD, Frankville DD; North American Pediatric Spine Anesthesiologists Investigators (Moore RP). A survey of practice in the anesthetic management of adolescent idiopathic scoliosis spine fusion by the North American Pediatric Spine Anesthesiologists Collaborative. Paediatr Anaesth. 2024 Jul;34(7):645-653
Recent Presentations
- Mavarez-Martinez A, Al-Bizri E, Tateosian VS . Transversus Abdominus Plane Block in Neonates: An Underutilized Approach for PostOperative Pain Management. Perioperative Medicine Summit, Orlando Mar 2020
- Mavarez-Martinez A, Tateosian VS . Comparison of Simulation with Problem Based Learning Discussions for Anesthesia Training. IARS 2020
- Figueroa C, Bracero L, Jacob Z. Quick Recognition And Management of Tension Pneumothorax In A Neonate With Trisomy 18 Under General Anesthesia. ASA 2021
- Kang RS, Kim Y, Tateosian V. Perioperative Management of a Patient with Heterotaxy Syndrome. ASA 2021
- Watson E, Usama S, Moore R. Coordinated Tumor Manipulation and Ventilation in a Pediatric Endobronchial Lesion with Intermittent Airway Occlusion. ASA 2021
- Mathew A, Watson E, Guyen V, Tateosian V. Airway Challenges In a Neonate With Congenital Epulis. PGA 2021
- Kang RS, Christophides A, Mena S, Tateosian V. Foreign Body Detected During Magnetic Resonance Imaging: A Case Report. IARS 2022
- Christophides A, Poghosyan V, Tateosian V. Perioperative morbidity within the incubation period of COVID-19 infection. IARS 2022
- Hafeman M, Poghosyan V, Ahmad SM, Tateosian V. Perioperative morbidity in a child with severe obstructive sleep apnea. IARS 2022
- Figueroa C, Zerrahn Z, Jasiewicz RC. Recurarization in an 8-week-old Infant Following Suggamadex Reversal of Rocuronium. ASA 2022
- Hafeman M, Desai AG, Moore RP. High Thoracic Erector Spinae Plane (ESP) Block for Humeral Osteotomy. ASA 2022
- Kozlowski P, Turkiew E, Desai AG, Bennici LA, Moore RP. Opioid Free Thoracolumbar Fusion in a Pediatric Patient with a Polysubstance Abuse History. ASA 2022
- Turkiew E, Kozlowski P, Moore RP. Application of a Hybrid Perioperative Medical-surgical Home Model to Achieve Care Goals for a Complex Pediatric Patient. ASA 2022
- Christophides A, Redmond V, Tateosian VS. Anesthetic Management of Pediatric Cerebral Aneurysm Intervention. ASA 2022
- Christophides A, Redmond V, Tateosian VS. Preoperative Predictors of Postoperative Complications in the Pediatric Population with Obstructive Sleep Apnea. ASA 2022
- Crugnola W, Costa A, Abola R, Al-Bizri E. Institutional Prevalence Of Sugammadex Use In Pediatric Patients. PGA 2022
- Lee C, Kozlowski P, Al-Bizri E. Axillary Nerve Block To Aid In Recovery Of Ischemic Limb In 5-Month-Old. PGA 2022
- Kozlowski P, Corrado T, Al-Bizri E. Carotid Artery Injury Caused By A Metal Sipping Straw In A Pediatric Patient. PGA 2022
- Rahman S, Desai A, Moore R. Erector spinae plane block for cancer related brachial plexus pain - A new role for regional anesthesia in NORA? ASRA 2023
- Singh N, Ahn J, Chen X, Park S, Hsieh H, Moore RP. Improved Post Operative Outcomes with ERAS protocol in the Pediatric Ambulatory Surgical Population. World ERAS Congress May 2023
- Khan A, Oster S, Khan M, Olsen P, Li K, Hsieh H, Romeiser J, Noll E, Moore RP, Bennett-Guerrero E. Insights from the child’s perspective - validation of a pictorial version of the quality of recovery-15 (qor-15 peds) questionnaire. American Society for Enhanced Recovery Meeting- September 2023
- Singh N, Ahn J, Chen X, Park S, Cardamone S, Davis R, Hsieh H, Moore RP. Improved post-operative outcomes and reduced narcotic use with eras protocol in a pediatric ambulatory surgery setting. American Society for Enhanced Recovery Meeting- September 2023
- Rahman S, Desai A, Moore R. Erector spinae block for NORA to treat selective brachial plexus pain in patient with metastatic lung cancer. PGA 2023
- Chernoff D, Jin Z, Tsivitis A, Al-Bizri E. Single Shot Fascia Iliaca Plane Block for Femur Fracture in a Pediatric Trauma Patient. PGA 2023
- Tsivitis A, Kozlowski P, Corrado T, Chesler D, Moore R, Al-Bizri E. Traumatic carotid artery injury caused by a metal sipping straw in a pediatric patient: Anesthetic management and considerations. Soc Ped Anes 2024
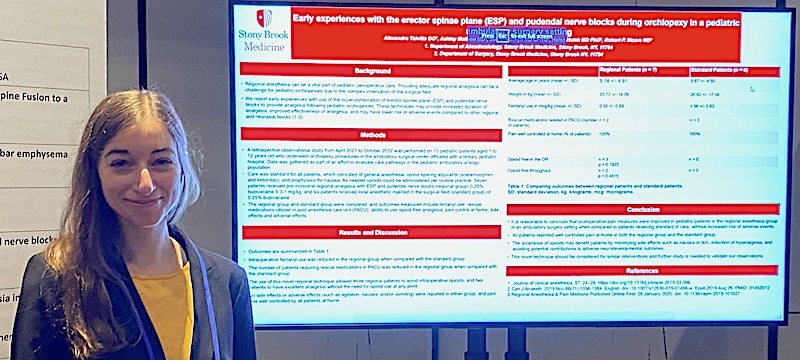
- Tsivitis A, Mathew A, Singh S, Hsieh H, Moore RP. Early experiences with the erector spinae plane (ESP) and pudendal nerve blocks during orchiopexy in a pediatric ambulatory surgery setting . Soc Ped Anes 2024