The Division of Cardiothoracic Anesthesiology is comprised of faculty members whose clinical practice focuses on patients undergoing cardiac and thoracic procedures in the operating room and catheterization laboratory. Our continued mission is to offer safe, uncompromising, elite-level care for patients undergoing these procedures, while providing the highest quality educational environment to our residents and medical students.
Division Members

- Derek Atkinson, MD joined our team in 2018 after completing a Fellowship in Cardiothoracic Anesthesiology at Columbia University. He has special interest in thoracic anesthesiology and is conducting research as the director of the Enhanced Recovery Program for Thoracic Surgical Procedures.
- Adrian Fischl, MD joined our team in 2019 after completing a Fellowship in Cardiothoracic Anesthesiology at Penn State University. He is the director of multiple Enhanced Recovery Programs within the department.
- Igor Izrailtyan, MD joined our team in 2005 after completing a Fellowship in Cardiothoracic Anesthesiology at Duke University Medical Center. He is the director of the Perioperative Echocardiography Service and leads the quality improvement initiative for our TEE program.
- Jeremy Poppers, MD, PhD, FASE is the Chief of Cardiothoracic Anesthesia Division. He completed his Fellowship in Cardiothoracic Anesthesiology at Brigham and Women's Hospital/Harvard Medical School in 2009 and joined the department as Chief of the division in 2015. He has special interest in the clinical applications of quantitative 3D TEE and has been recognized for his teaching in cardiac anesthesiology and TEE.
- Giacomo "Jack" Scorsese, DO joined our team in 2024 after completing a Fellowship in Cardiothoracic Anesthesiology at The Icahn School of Medicine at Mount Sinai. His areas of interest are complex mitral valve surgery, mechanical circulatory support in advanced heart failure and the use of regional anesthetic techniques for cardiac surgery.
- Christopher Seiter, DO joined our team in 2024 after completing a Fellowship in Cardiothoracic Anesthesiology at Vanderbilt University Medical Center. His clinical interests include complex open & endovascular aortic surgery, as well the use of 3D echocardiography for structural heart interventions.
- Eric Zabirowicz, MD joined our team in 2015 after completing a fellowship in Cardiothoracic Anesthesiology at Columbia University Medical Center. He is the Section Chief of TEE/EP. He has a special interest in surgical treatments for heart failure and mechanical circulatory support.
Residency Training
During their cardiothoracic rotation, residents are exposed to a wide variety of cardiac and major aortic cases, including on- and off-pump coronary revascularization surgery, valve repair and replacement, aortic aneurysm and dissection repair. In addition, residents will gain experience in caring for patients with advanced heart failure who require placement of mechanical assist devices such as intra-aortic balloon pumps, ventricular assist devices (VADs) and extra corporeal membrane oxygenation (ECMO). Residents will also gain familiarity with patients undergoing trans-catheter aortic valve replacements (TAVRs) and a multitude of thoracic surgical cases, including pulmonary and esophageal resections.
Residents rotate through the cardiothoracic division for a month-long block starting in the middle of their CA1 year. Additional weeks on the service assigned during their CA-2 and CA-3 years. During their rotation, residents will become proficient in the placement of arterial, central venous and pulmonary artery catheters, double lumen endotracheal tubes and bronchial blockers. Transesophageal echocardiography (TEE) experience will be acquired intraoperatively as well.
In addition to a diverse clinical experience, the cardiothoracic rotation offers a structured didactic program, comprised of a series of faculty lectures. Our faculty are genuinely excited to teach our residents, as well as serve as mentors for residents who wish to pursue academic projects, ranging from clinical research to challenging case reports, during the course of their rotation and residency; our residents have traditionally presented abstracts and complex cases at regional and national meetings.
Residents rotate through the cardiothoracic division for a month-long block starting in the middle of their CA1 year. Additional weeks on the service assigned during their CA-2 and CA-3 years. During their rotation, residents will become proficient in the placement of arterial, central venous and pulmonary artery catheters, double lumen endotracheal tubes and bronchial blockers. Transesophageal echocardiography (TEE) experience will be acquired intraoperatively as well.
In addition to a diverse clinical experience, the cardiothoracic rotation offers a structured didactic program, comprised of a series of faculty lectures. Our faculty are genuinely excited to teach our residents, as well as serve as mentors for residents who wish to pursue academic projects, ranging from clinical research to challenging case reports, during the course of their rotation and residency; our residents have traditionally presented abstracts and complex cases at regional and national meetings.
Recent Division Activity
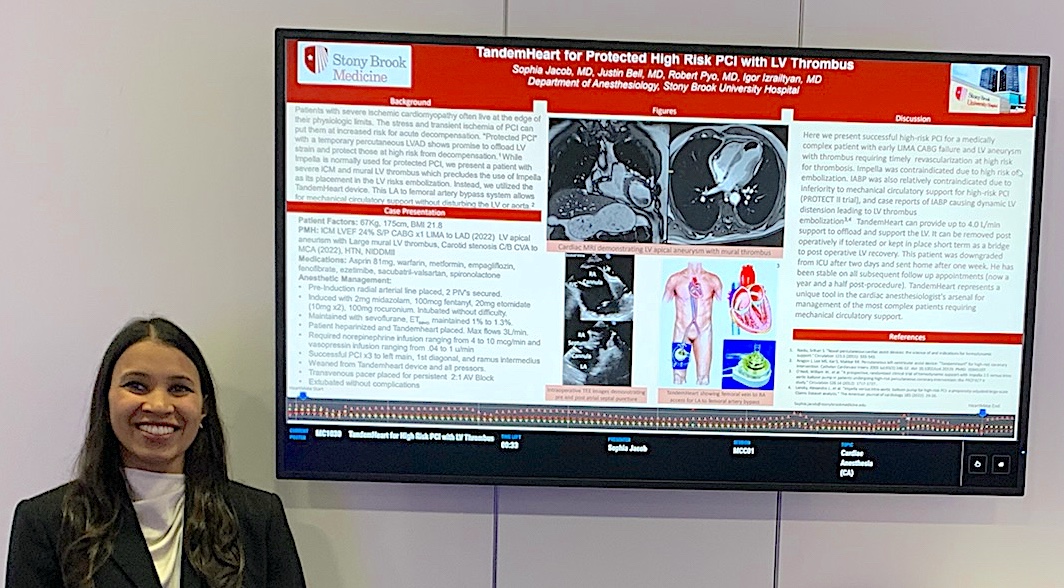 Resident Dr. Sophia Jacob presenting at the 2023 ASA meeting |
 |
Recent Publications
Resident authors denoted by bold type
- Izrailtyan I, Poppers J, Kowal R, Zabirowicz E, Nie L, Gan TJ, Bennett-Guerrero E. Comprehensive Quality Improvement Program for Intraoperative Transesophageal Echocardiography: Development, Implementation, and Initial Experience. J Cardiothorac Vasc Anesth. 2020 Aug 7.
- Parikh PB, Romeiser JL, Dhautel B, Mitchell D, Holecek W 3rd, Bilfinger T, Poppers J, Bennett-Guerrero E. Predictors and impact of low diastolic blood pressure and widened pulse pressure following transcatheter aortic valve replacement. Cardiovasc Revasc Med. 2021 Oct 28.
- Shuaib K, Scorsese G, Seiter C, Zabirowicz E, Poppers J. Diagnosis and Management of a Unique Iatrogenic Biatrial Gerbode Defect. Case Rep Anesthesiol. 2022 Jul 18.
- Scorsese G, Hake A, Christophides A, Poppers J, Zabirowicz E. Anesthetic Management of a Large Right Ventricular Mass due to Idiopathic Hypereosinophilic Syndrome in a Patient Undergoing Cardiac Surgery, a Case Report. Semin Cardiothorac Vasc Anesth. 2022 Oct 7.
- Atkinson DJ, Romeiser JL, Almasry IO, Tannous HJ, Parikh PB, Bennett-Guerrero E. Randomized controlled trial of liberal vs. standard fasting instructions in percutaneous cardiac procedures. Perioper Med (Lond). 2023 Aug 8;12(1):44.
- Conen D, et al; COP-AF Investigators (including Poppers J). Effect of colchicine on perioperative atrial fibrillation and myocardial injury after non-cardiac surgery in patients undergoing major thoracic surgery (COP-AF): an international randomised trial. Lancet. 2023 Nov 4;402(10413):1627-1635.
- Mattimore D, Fischl A, Christophides A, Cuenca J, Davidson S, Jin Z, Bergese S. Delirium after Cardiac Surgery-A Narrative Review. Brain Sci. 2023 Dec 7;13(12):1682.
- Bargnes III V, Davidson S, Talbot L, Jin Z, Poppers J, Bergese SD. Start Strong, Finish Strong: A Review of Prehabilitation in Cardiac Surgery. Life 2024, 14(7), 832.
Recent Presentations
- Shah R, Katz S, Atkinson D. Severe Post-induction Bronchospasm in a Patient with Atypical Carcinoid Tumor. ASA 2020
- Parsey D, Shuaib K, Watson E, Schwartz J, Kowal RA, Poppers JS. Diagnosis and Management of Unique Gerbode Defect Variation Consisting of a Bi-atrial Regurgitant Jet At the Base of the Inter-atrial Septum Originating From the Left Ventricular Outflow Tract. ASA 2020
- Alam S, Tenure RS, Poppers JS. LA Thrombus Formation on An Amplatzer Occluder Device in a Patient with Factor V Leiden on Dabigatran. ASA 2020
- Shuaib K, Angelo T, Poppers J, Factor M. Anesthetic Considerations in a Parturient with Complex Cardiac History and Pulmonary Hypertension. PGA 2020
- Kozlowski P, Christophides AH, Izrailtyan I. To Sedate Or Intubate? A Case Report Highlighting The Anesthetic Management Of Cardiac Tamponade. ASA 2021
- Mathew A, Christophides AH, Balaguer JM, Izrailtyan I. Bilateral Abnormal Ultrasound Allen Test: A Management Dilemma. ASA 2021
- Xiao A, Tai J, Christophides A, Gavalas M, Price L, Sun E, Izrailtyan I. Do No Harm: Intraoperative Management Of An Unstable Patient Undergoing Multiple Procedures. ASA 2021
- Scorsese G, Poppers J. Native Valve Infective Endocarditis Causing Intraoperative Acute Limb Ischemia. ASA 2021
- Seiter C, Kim B, Zabirowicz E, Poppers J. Anesthetic Considerations And Alternatives For A Patient With Severe Hypertrophic Cardiomyopathy Presenting For Orthopedic Surgery. ASA 2021
- Mena S, Poppers J, Zabirowicz E. Severe Mitral Valve Regurgitation After Tricuspid Valve Replacement. PGA 2021
- Kang R, Cuenca J, Landau D, Schulsinger D, Izrailtyan I. Anesthetic Management of a Patient with an Infected Aortic Graft. ASA 2022
- Cuenca J, McLarty A, IIzrailtyan I. Mechanical Circulatory Support for High-risk Coronary Artery Bypass Grafting. ASA 2022
- Scorsese G, Hake A, Balaguer J, Izrailtyan I. Anesthetic Management and Considerations in Prosthetic Valve Endocarditis. ASA 2022
- Shafai A, Williams R, Dhamija A, Izrailtyan I. Intercostal Cryoablation for Post-Thoracotomy Pain. ASA 2022
- Zhu M, Dhamija A, Sasson A, Izrailtyan I. Successful Intubation of Patient with Obstructive Squamous Cell Carcinoma with the Assistance of an Airway Exchange Catheter. ASA 2022
- Cuenca J, Scorsese GF, Poppers JS. Left Main Coronary Artery Disease Complicated by Retroperitoneal Hemorrhage with Mixed Hemorrhagic, Cardiogenic and Septic Shock. ASA 2022
- Scorsese G, Rakhamimova E, Poppers JS. Anesthetic Management and Considerations for Debakey Type I Aortic Dissection in a Jehovah's Witness. ASA 2022
- Jacob S, Bell J, Pyo R, Izrailtyan I. TandemHeart for High Risk PCI with LV Thrombus. ASA 2023
- Fardos Y, Elias M, Beg T, Poppers JS. Diagnosis and Management of Intraoperative PE during Orthopedic surgery requiring ECMO. ASA 2023
- Hum B, Lee C, Zhang K, Hafeman M, Atkinson DJ. Management of Cardiac Tamponade Following Incidental Puncture of Pericardium During Mechanical Thrombectomy. ASA 2023
- Kim E, Elias M, Atkinson DJ, Poppers JS. Perioperative Management of a Patient with C1-esterase Inhibitor Deficiency Undergoing Cardiac Surgery. ASA 2023
- Jacob S, Bell J, Pyo R, Izrailtyan I. TandemHeart for High Risk PCI with LV Thrombus. ASA 2023
- Elias M, Kim EK, Zabirowicz E. Perioperative Management of a Patient with Factor VII Deficiency Undergoing Cardiac Surgery. ASA 2023
- Chen S, Balaguer J, Izrailtyan I, Mattimore D. A Case of Suspected Left Ventricular Wall Perforation after Intraoperative IMPELLA® Insertion. PGA 2023
- Hum B, Fischl A, Lee C, Shibly Y, Zhang K. Management of Severe Pulmonary Hypertension During Open Inguinal Hernia Repair Under Epidural. PGA 2023
- Mattimore D, Chen S, Ahn J, Price J, Poppers J. Delayed Coronary Obstruction Presenting as Myocardial Infarction 5 Years After Transcatheter Aortic Valve Replacement. SCA 2024
- Jin Z, Rakhamimova E, Christophides A, Poppers J. Parasternal intercostal nerve block for analgesia in surgeries requiring sternotomy, a systematic review and meta-analysis. ASA 2024
- Bargnes V, DiMaria S, Cuenca J, Yammine M, Poppers J. Triple Valve Cardiac Surgery with Bovine Aortic Valve Replacement, Maze Procedure, and Left Atrial Appendage Clipping in a Patient with Alpha-Gal Syndrome. ASA 2024
- Singh S, Bolze E, Fischl A, Sasson A, Bennett-Guerrero E. Employing a Novel Datamart to Monitor Surgical Oncology Enhanced Recovery Program. ASA 2024
- Li D, Li TM, Fischl A, Murphy J, Kim C, Bergese S. Quantitative Analysis of Prothrombin Complex Concentrate Clinical Trials Reveals Extreme Sex Bias. ASA 2024
- DiMaria S, Li J, Cuenca J, Fischl A. Management Of Acute Cardiogenic Shock Secondary To Viral Myocarditis Using Mechanical Circulatory Support. ASA 2024
- Espeleta J, Bargnes V, Fischl A. Don’t Be Conned by Primary Hyperaldosteronism: Anesthetic Considerations for Conn Syndrome. PGA 2024
- DiMaria S, Li J, Cuenca J, Fischl A. Management Of Acute Cardiogenic Shock Secondary To Viral Myocarditis Using Mechanical Circulatory Support. PGA 2024
- Davidson S, DiMaria S, Bargnes V, Feit A, Poppers J. VV ECMO to the Rescue: Successful Recovery from Refractory Intraoperative Anaphylaxis Following Redo Sternotomy for Mitral Valve Replacement. PGA 2024
- Yerramalli G, Bargnes V, Oster J, Atkinson D, Poppers J. Patient with Heparin-Induced Thrombocytopenia having Adverse Reactions to Heparin having Mitral Clip Placement for Severe Mitral Regurgitation. PGA 2024
- Tsivitis A, Atkinson D, Nguyen N, Feit A. Urgent laparotomy and salpingectomy secondary to ectopic pregnancy in a patient requiring VA ECMO after V fib arrest at home. PGA 2024
- Fiola J, Park G, Price J, Izrailtyan I. Operative Management in Setting of Anomalous Origin of Coronary Artery. PGA 2024
- Shibly Y, Bargnes V, Tannous H, Izrailtyan I. An Urgent CABG Complicated by Coronary Artery Intramural Hematoma from Percutaneous Intervention with Corresponding Electrocardiogram and Echocardiogram Changes in the Setting of Renal Transplantation. PGA 2024
- Lin K, Bargnes V, Bodily S, Elias M, Epstein R, Zabirowicz E. Topicalization & TIVA: A Successful Anesthetic Duo for Endobronchial Oxidized Cellulose Placement in the Treatment of Bronchopleural Fistula. PGA 2024