| Residency Program Inquiries | updated: 11-19-25 |
- Visit our Instagram and X pages!
- CA-3 Resident Dr. Genna Monanian was selected for induction into the Alpha Omega Alpha (AΩA) Honor Society! This prestigious honor reflects her outstanding academic and clinical achievements, and her embodiment of the core principles that AΩA represents: scholarship, leadership, professionalism, service, and dedication to the art of teaching and education.
- CA-3 Resident Dr. Vince Bargnes was named the recipient of the 2025 American Society of Anesthesiology (ASA) Resident Distinction Award! This is ASA's highest national honor for anesthesiology residents, indicating a superior level of service, leadership, advocacy, and education.
- CA-3 Resident Dr. Alexandra Tsivitis was named the recipient of the 2025 American Osteopathic College of Anesthesiologists (AOCA) Resident of the Year! This is the AOCA’s highest national honor for anesthesiology residents, indicating remarkable scholarship, leadership, and dedication to the osteopathic profession.
- CA-2 Resident Dr. Bill Crugnola received recognition for the ABA for his top 10% performance on the 2025 ABA Basic Exam
- CA-2 Resident Dr. Stephen DiMaria received recognition for the ABA for his top 10% performance on the 2025 ABA Basic Exam
- CA-3 Resident Dr. Alexandra Tsivitis will be a Pediatric Anesthesiology fellow at the University of Pittsburgh for 2026-2027.
- CA-3 Resident Dr. Genna Monanian will be an Obstetric Anesthesiology fellow at Stony Brook University for 2026-2027.
- CA-3 Resident Dr. Sophia Jacob will be an Obstetric Anesthesiology fellow at Mount Sinai West, NY for 2026-2027.
- CA-3 Resident Dr. Vincent Bargnes was elected as Junior Co-Editor of ASA Monitor’s Residents’ Review.
Choose Stony Brook!

Class of 2029
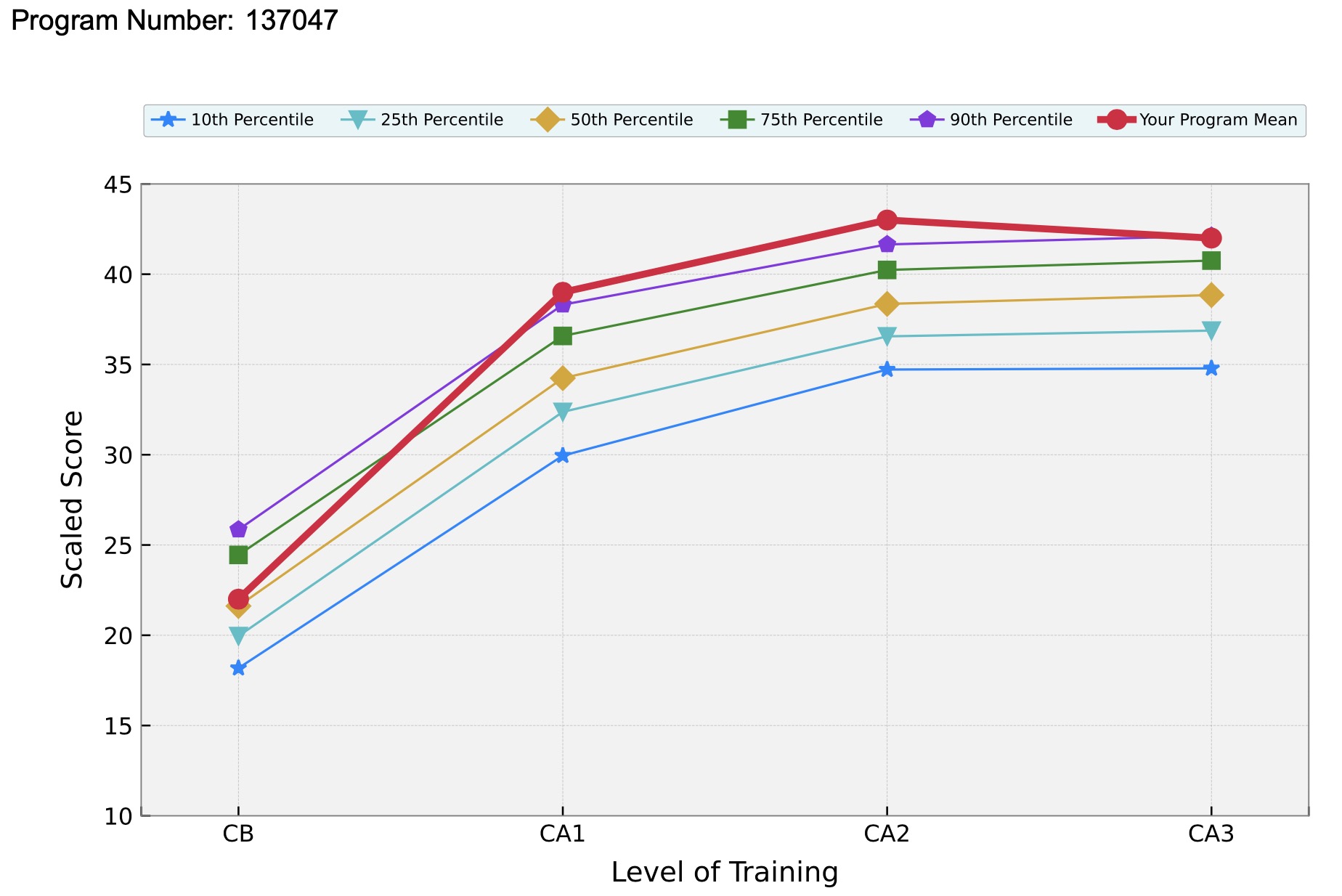
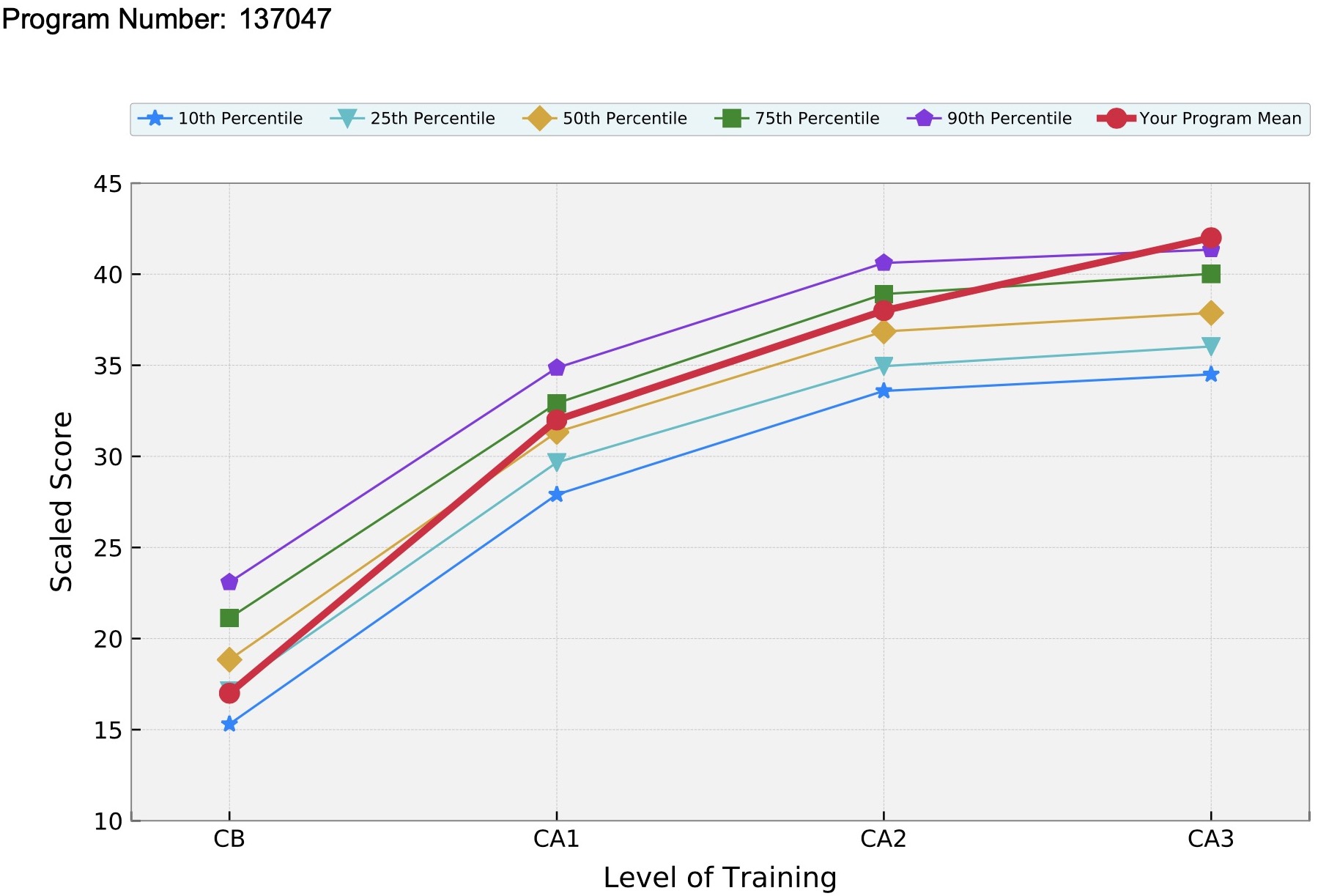
Our program's impressive annual in-training exam performances (2025 CA3 report) reflect the exceptional training and educational resources provided in our residency program. The end product of this anesthesia residency education is a superbly trained consultant in anesthesiology, able to provide the highest quality of care to patients in the most challenging clinical conditions.
Leapfrog awarded Stony Brook University Hospital a grade of "A" for hospital safety, Fall 2024. Healthgrades named Stony Brook Medicine as one of “America’s 50 Best Hospitals™" for 2025! This puts us in the top 1% of hospitals in the nation for exhibiting clinical excellence year over year. [Read more]
"What To Expect As A Resident" with CA-2 Dr. Genna Monanian
|
Residency Program At-a-Glance
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
▶ Welcome Messages
▶ 2025-26 Interviews
All residency interviews will be virtual in 2025-26. Applicants need to have completed USMLE Step 1 and Step 2 to be considered for an interview.
▶ ABA Basic Exam
Several of our residents perform at or above the top 10% nationwide on the ABA Basic Exam that is taken at the end of CA1 year. These residents receive special recognition from the ABA for their top 10% performance. Congrats to CA2s Drs. Crugnola and DiMaria for their outstanding top 10% performance in June 2025!
 ▶ Academic Mentorship Program
Our Academic Mentorship Program (AMP) creates a productive and efficient academic infrastructure to promote resident involvement and leadership in academic activities. Our Research Chief Resident liaisons with faculty who provide mentorship on academic and research endeavors to junior residents. Most projects lead to publication and/or conference presentations.
 ▶ ACGME Milestones
▶ Annual In-training Exam Performance
2025 CA3 Intraining Exam Performance (click graph to see full report)
2023 Intraining Exam Performance (click graph to see full report) 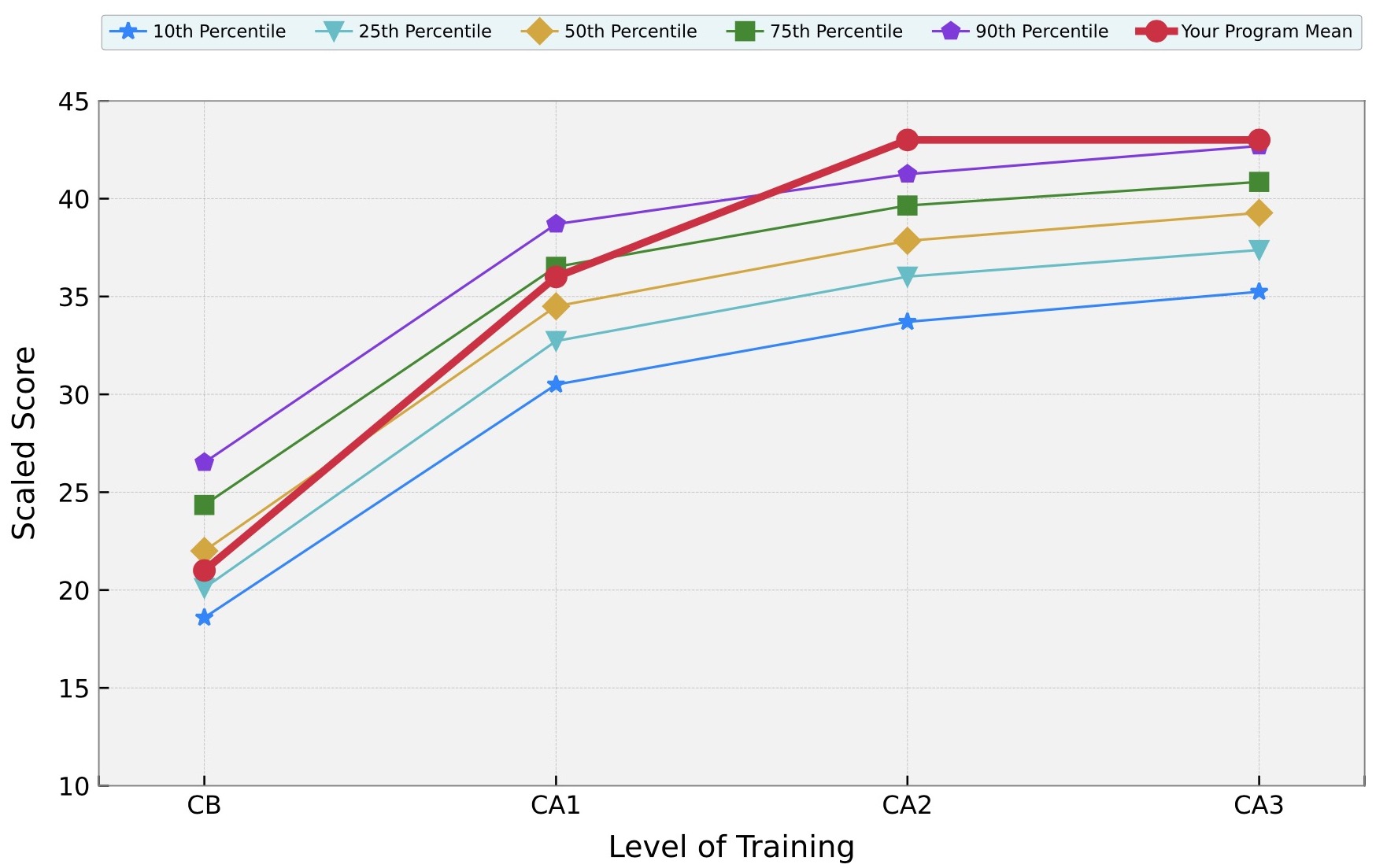
2022 Intraining Exam Performance (click graph to see full report) 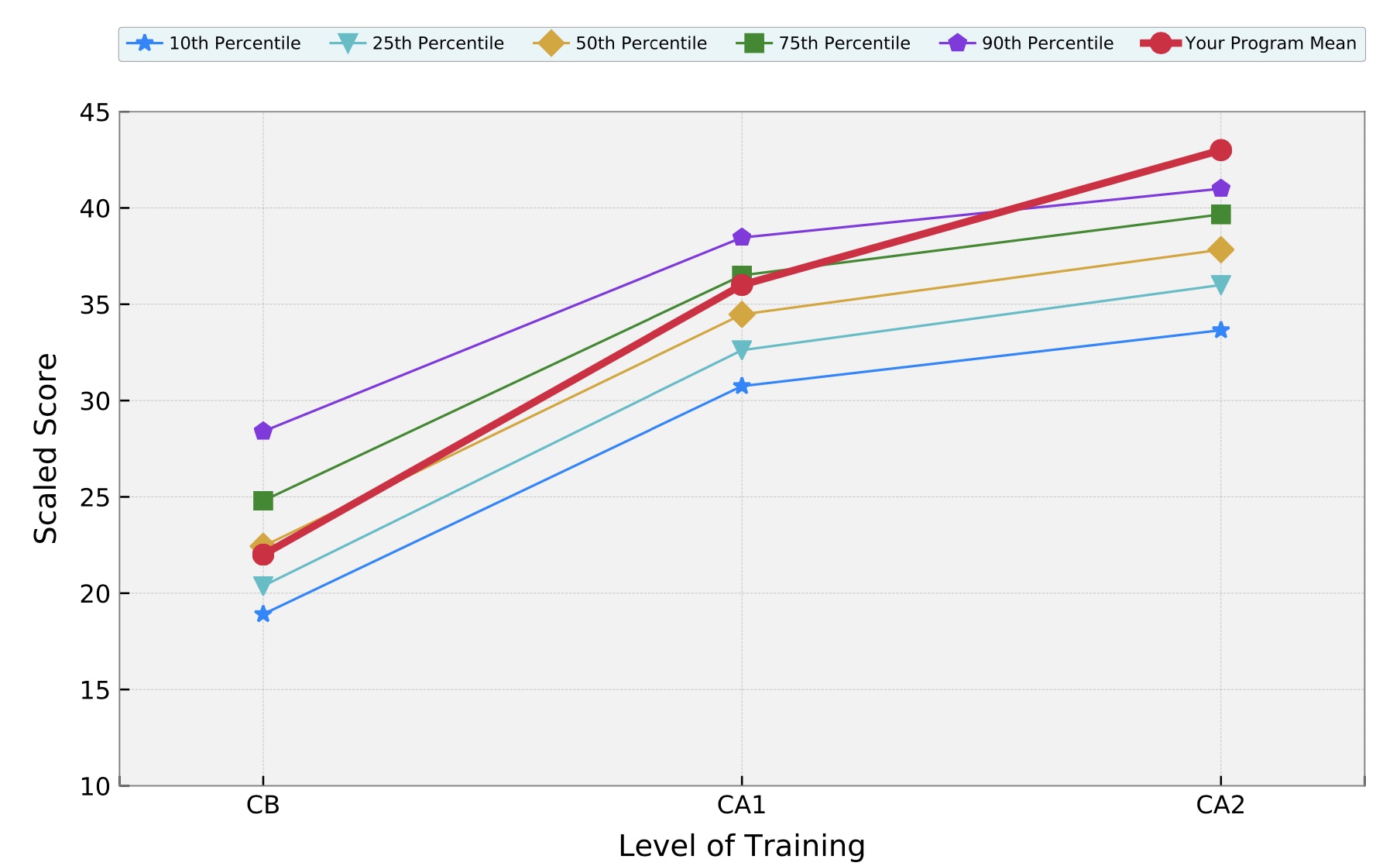
2021 Intraining Exam Performance (click graph to see full report) 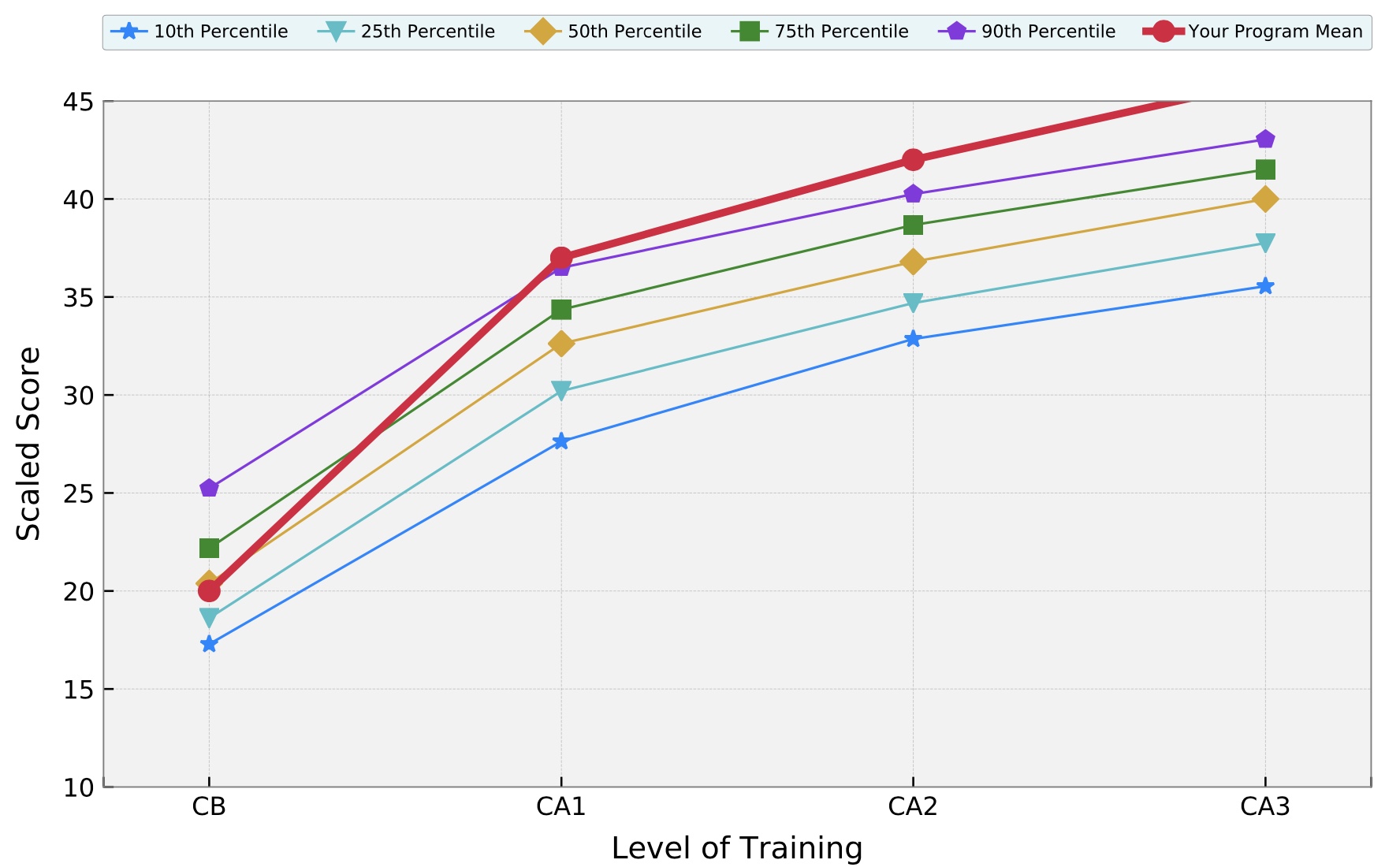
2020 Intraining Exam Performance (click graph to see full report) 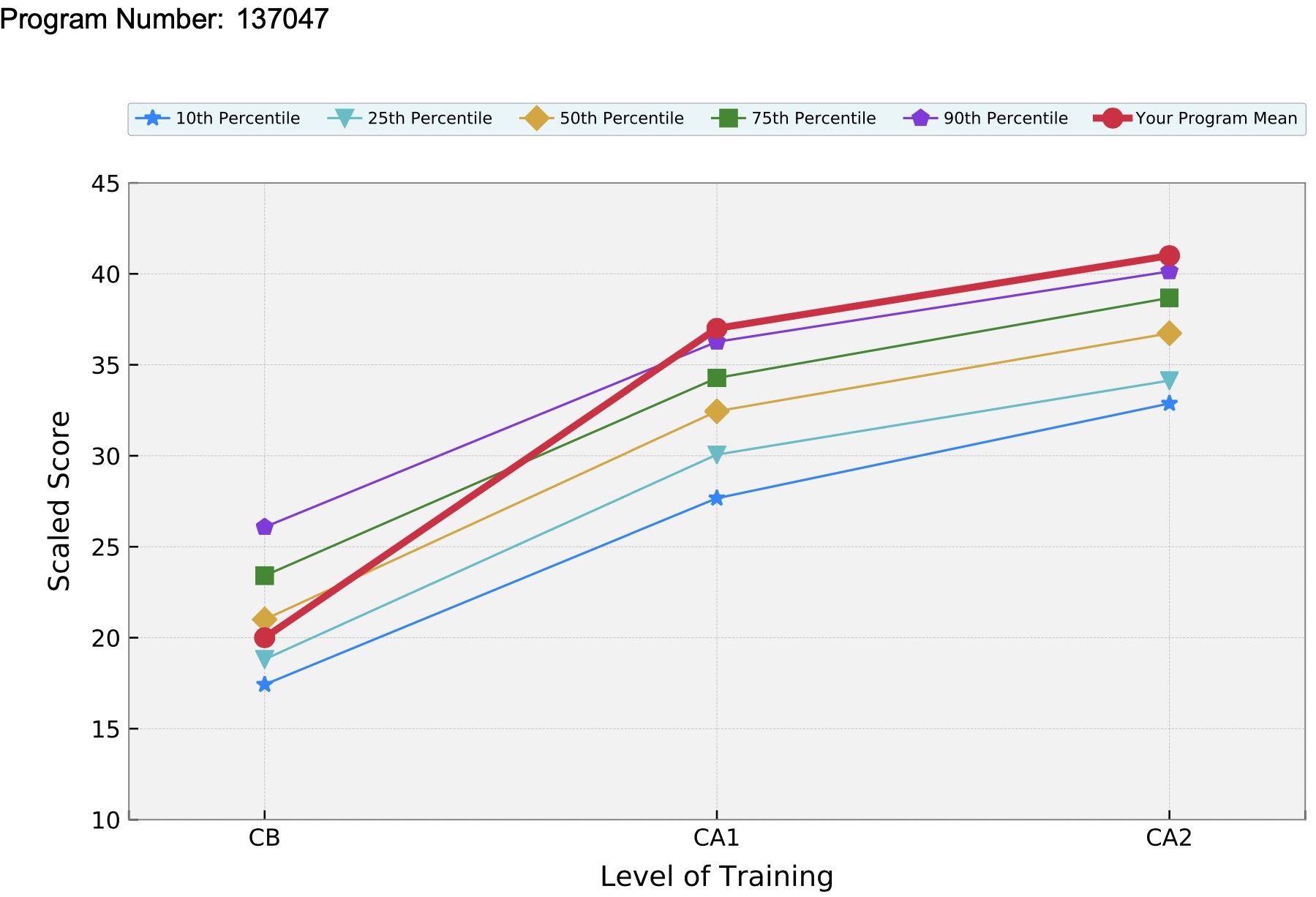
▶ ASA and NYSSA Resident Leadership

Congratulations to CA2 Dr. Seth Greenspan for serving on the ASA House of Delegates Reference Committee for Scientific Affairs. Congratulations to CA2s Drs. Greenspan, Mangano and CA1 Dr. Yep for being appointed to leadership positions within the New York State Society of Anesthesiologists ( NYSSA). They were also selected as NYSSA Delegates for the ASA Resident Component House of Delegates. They will be official voters for NY state on national resident-specific issues and will select the ASA Resident Component Governing Council. Let’s go Vince, Seth, Nick and Hannah! ▶ Chief Residents 2025-2026
▶ Clinical Base Year
The Stony Brook Anesthesiology Residency Program is a four-year program. During the clinical year (PGY- 1), our interns rotate through the Emergency Room, Surgery, Medicine, MICU, Echo, OB and Anesthesiology and have introductory experiences in acute and chronic pain assessments management. They also have a two-week Patient Safety rotation.

Class of 2029
▶ Clinical Divisions and Rotations
The department is organized into clinical Divisions that emphasize the many subspecialties of anesthesiology.
Use the links below to meet the members of each Division, learn about their academic and research activities, and discover what a Day-in-the-Life-of-a-Resident is like! ▶ Clinical Skills Center and Simulation

Simulation is a component of our residents’ educational experience. There are numerous values to simulation. These include standardization of education, allowing residents to have their medical decisions proceed to a logical conclusion without attending intervention, identification of weaknesses in knowledge base as well as improving technical ability and learning through a kinesthetic teaching process. The Clinical Skills Center at Stony Brook Medicine is a 4,000 square foot state-of-the-art training center that can be used as a resource for specialized training of physicians and other healthcare professionals. The Department of Anesthesiology has played a critical role in this Center from its inception. An operating room, complete with a high fidelity mannequin and a realistic setting, makes this an exciting educational experience. The majority of the Wednesday teaching sessions include a simulator component. The simulator is used to create rare and dangerous situations that the resident may never see during the course of a residency. Examples include airway fires, malignant hyperthermia, anaphylaxis and the incapacitated surgeon. In addition, more routine types of cases and complications can be taught in the simulator, so the resident can encounter such scenarios as “cannot intubate, cannot ventilate” or serious arrhythmias in a safe environment. They can practice clinical skills such as intubate and placing lines on mannequins instead of “real patients”. ▶ Clinical Training
From the outset, the department has maintained a fully accredited residency training program. We are a four-year program. The Clinical Base Year (CBY) consists of rotations in the Departments of Medicine, Surgery and Emergency Medicine, including 10 weeks of medicine, 8 weeks of MICU, 12 weeks of surgery, 4 weeks in the Emergency Room, 2 weeks of OB, 4 weeks in Anesthesiology and 2 weeks Intro to Acute Pain, 1 week Intro to Chronic Pain, 1 week ECHO and 2 weeks Patient Safety. The CBY residents will have the opportunity to interact with faculty and residents in the Department of Anesthesiology.
Three groups of residents undergo training in each of the three clinical anesthesia years of training (CA-1, 2 and 3 years equivalent to PGY 2, 3 and 4). There is large variety in a very substantial caseload. All specialties and subspecialties are represented. All anesthetics are delivered by residents under the direction of an attending anesthesiologist. This supervision is given 24 hours per day, either on a one-to-one basis or, at most, in a ratio of one attending for two residents. It is an expression of our standard: optimal care, for all patients, at all hours. This applies not only in the operating rooms, but also in the obstetrical delivery suite, the intensive care units and the pain clinic. This clinical instruction may be strenuous and demanding; it is alleviated by the strong personal relationship between attending and resident and by certain amenities, such as breaks throughout the working day, an attending late call system to allow timely resident relief, education days that break up the clinical routine and wellness sessions to provide self-care education and social support. In addition, we have a night float call system. Residents on OR night float are off on all weekends for the rotation. Weekend call for other rotations averages 1-2 weekends/resident/month. Duty hours range from 50-55 hours/week if not on weekend call, 65-74 hours/week if on weekend call. ▶ Clinical Training Sites
▶ Community Outreach
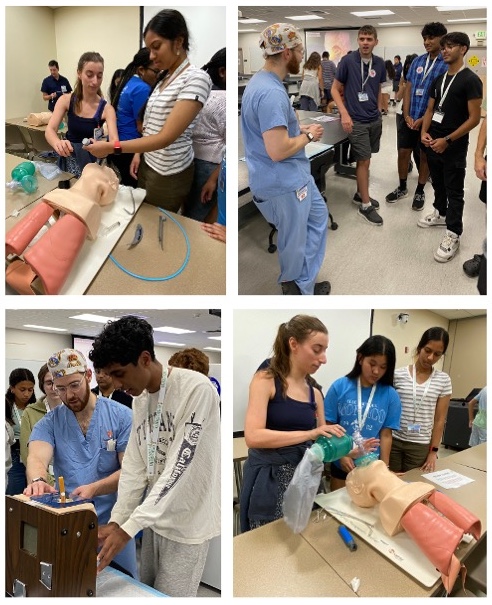
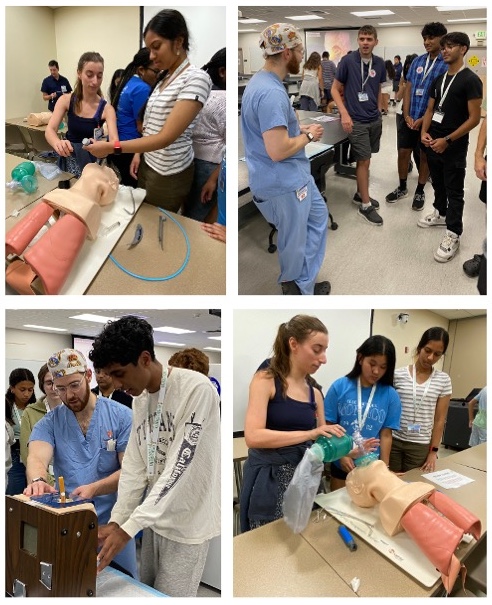
Science and Research Awareness Series (SARAS) is a 3-week, summer program designed to heighten the awareness of High School and Undergraduate students in many aspects of Biomedical Science. The program is sponsored by the Department of Anesthesiology and directed by Dr. Srinivas Pentyala. Many of our faculty members, residents and medical students participate in SARAS lectures and workshops. SARAS has been offered since 2004 and typically attracts over 100 participants, including high school students from backgrounds underrepresented in medicine.
Dr. Ursula Landman, Associate Professor of Anesthesiology, is the Walk Leader for the Stony Brook Medicine Chapter of “Walk With a Doc”. They sponsor monthly walks at a local park (or virtually during the pandemic, or at a local mall in inclement weather). The “Walk with a Doc” walks are a way to inspire our community through movement and conversation. It’s aim is to make hope and health accessible to all. Doctor led walks are a safe, fun, and a FREE place to get some steps in, learn about health and careers in medicine, and meet new friends. 
▶ Diversity and Inclusion
The Department of Anesthesiology at Stony Brook University Hospital is committed to building an inclusive culture that celebrates the diverse voices in our residents, faculty and staff. We do not discriminate based on race, sex, gender, religion, ethnicity, disability, citizenship, or any other values that makes us each unique. The voices of our different viewpoints and perspectives, backgrounds, and experiences are valued.

We celebrate diversity and seek to promote the inclusion of everyone in our residency program. Our residents, faculty, students, support staff and patients represent a wide range of countries, cultures, socio-economic backgrounds, and sexual identities, all which reflect and enhance our medical community and all those whom we serve. For further information on how our institution is committed to inclusion and diversity, please visit: https://renaissance.stonybrookmedicine.edu/gme/diversity_inclusion. The Department of Anesthesiology and Stony Brook Medical Center partnered with the American Medical Association (AMA) in their shared commitment to dismantling structural racism and increasing diversity in the physician workforce. Members of the Department of Anesthesiology participate in the annual Stony Brook “Black Men in White Coats” Youth Summit. Over 500 youth from backgrounds underrepresented in medicine attend the event. Black Men in White Coats is an AMA-created documentary that inspires to increase the number of Black men in the field of medicine. During the summit, participants examined the structural barriers to increasing diversity in medicine from the perspectives of Black men who are both physicians and leaders in medicine. Photos and videos from the 2024 Summit.  CA1 Resident Dr. Bintia Sakho with some of the participants at the 2025 Summit ▶ Education
Wednesday 7 AM Conferences
Wednesday 8:00am- 3:00pm Conferences (1 CA cohort per week; 1-2 times/month/CA class)
▶ Faculty


2024 Teachers of the Year. For residents: Dr. Daryn Moller, for medical students: Dr. Eman Nada Peer-reviewed publications Books and book chapters Teaching videos ▶ Fellowship Matches

40-60% of the graduates enter private practice Visit our Alumni page ▶ Global Health
Over the years, the Department of Anesthesiology has supported Residents and Attendings to participate in Global Health trips (Medical Missions). Recent destinations include Armenia, Zambia, The Philippines, Ecuador, China and Honduras.
Drs. Tateosian, Razak, Aravera and Ghaly on a Global Health trip to Armenia, May 2025 I went to Zambia during my last year of residency. I was so lucky to go - it was definitely an eye opener. I saw and learned SO much! it gave me a totally different perspective on medicine, how it can be done so differently with minimal resources. It forced me to get out of my comfort zone, and to still provide safe medical care. Now as an attending who is going on medical missions, I would recommend this experience to everyone! -Dr. Anna Kogan, former Stony Brook Resident and current Stony Brook Attending 
Ecuador Mission. Challenges: No consistent monitors, no emergency drugs available, finite amount of oxygen available, minimal equipment available. What we learned: You can work with less, not all propofol is created equal, you can reuse everything, turnover is faster without Joint Commission -Drs. Justin Smith and Minxi Wang, class of 2018. 
Dr. Kseniya Khmara (Class of 2018), Dr. Zvi Jacob, Dr. Michael Khalili (Class of 2019) ▶ GME Prospective Resident Webpage
Stony Brook Medical School's Prospective Residents and Fellows webpage provides information about Eligibility, Benefits, Salary, Housing, Policies, Inclusion and Diversity and more!
▶ GME Recognition

In honor of Resident and Fellow Appreciation Month (February 2025), Residents Drs. Adam Bindelglass (CA3), Genna Monanian (CA2), Seth Greenspan (CA1), and Catherine Devitt (PGY1) were selected for GME’s resident highlight page. ▶ Hospital Awards

Stony Brook Medicine has won numerous awards for clinical performance from Healthgrades.
The Division of OB Anesthesiology has been named a Center of Excellence by the Society of Obstetric Anesthesia and Perinatology. The SOAP Center of Excellence (COE) designation was created to recognize institutions and programs that demonstrate excellence in obstetric anesthesia care and to set a benchmark of expected care to improve standards nationally and internationally. 
The Maternity Ward was voted as Long Island's Best in 2021-2025. ▶ Journal Club
Journal Club is held every other month. Journal club is a didactic tool to teach lifelong learning skills. It is a way to keep current in the anesthesiology literature and to learn to read the literature with a critical eye.
Journal Club is organized and moderated by Eric Zabierowicz, M.D. All residents and faculty members have an opportunity to present at least once during the three year cycle. ▶ Leadership Training
Our residents gain clinical leadership experience by serving as the team leader when on call and also serving as the OR coordinator/floor runner during the day on a CA3 rotation. They learn to supervise junior residents, how to triage/prioritize cases/manage workflow, manage emergent airways, lead trauma anesthesia management and work as an attending in a busy clinical practice that has high acuity cases and residents and CRNAs.
For administrative leadership development, the residents have monthly “Chats with the Chair” where they have an opportunity to discuss topics related to leadership on a regular basis with the highest anesthesia leader in our medical center. The residents also receive a leadership didactic with our hospital CMO. We encourage our residents to pursue leadership roles locally, regionally and nationally since leadership is something that needs practiced to develop. Many of our residents serve on ASA Committees, NYSSA Committees, hospital, GME and departmental committees. This helps prepare them to be future leaders in the ASA or within their future practices. We provide them clinical coverage to attend the meetings that they need to attend. Our large CRNA work force helps us provide this coverage. Many of the hospital and GME committees are interdisciplinary. Lastly, during the PGY1 year, our interns have a 2-week Patient Safety Rotation were they are granted permission to attend high hospital-level administrative (CMO-level) meetings to learn how hospital leaders discuss and manage challenges within a health care system. 
The Academic Mentorship Program supported 12 abstracts at the 2024 ASA Annual Meeting ▶ Mentor Program
 Our program offers a formal Mentor Program where each resident is assigned to a faculty mentor at the start of the CA1 year. Residents may change their mentor if they like or they may obtain a second subspecialty faculty mentor. ▶ Mission Statement & Program Aims
Stony Brook Anesthesiology Residency Program’s Mission Statement: The mission of the Anesthesiology Residency Program at Stony Brook University Medical Center is to educate and facilitate the achievement of excellence in anesthesia care and thereby create physicians, who in the course of their careers, will play a role in improving the quality of healthcare in our nation through best practices, research, teaching and maintaining personal wellness. Enhanced Recovery After Surgery (ERAS) is a focus of our program's clinical mission to help ensure that patients in our local community have the best possible outcomes after surgery and to teach quality and patient-centered care practices to our residents. Our program's mission closely aligns with our institutional mission to provide state-of-the-art, safe and patient-centered care. Stony Brook Anesthesiology Residency Program Aims: The Stony Brook Anesthesiology Residency program has the primary goal of teaching and educating residents to become independent practitioners in the field of anesthesiology by offering a progressive and competency – based clinical experience, teaching the essential elements of research and quality care, and exposing them to the practices of physician well-being and medical education. This goal is achieved by providing a diverse patient population with various pathologies, a comprehensive didactic curriculum which includes learning through simulation, and a culture of inquiry to promote quality improvement, patient safety and scholarly activity. The training of Stony Brook Anesthesiology residents occurs in an environment of mutual respect which fosters the ability of residents to acquire the knowledge, skills, clinical expertise and experience to practice independently as an anesthesiologist in a compassionate and safe manner. Upon completion of the Stony Brook Anesthesiology Residency Program, residents are expected to: Patient Care
▶ Office-based Anesthesia
We provide exposure to Office based surgery. Residents rotate with an anesthesiologist where they are exposed to the isolated lonely environment of an office setting. This office is fully certified and offers the highest possible safety standards. This should prepare the residents to set the highest standards for themselves when they eventually are exposed to this growing arena.
▶ Operating Rooms
 Modern ORs with state-of-the-art equipment and capabilities ▶ POCUS Training
Our residents are enrolled in the ASA Diagnostic POCUS Certificate Program during their CA1 year. The department pays the individual resident’s program fee. Residents will complete the certification in 2 years or sooner. Residents will receive an ASA certificate of completion upon conclusion of the program.
We provide about 10 didactic lectures on Wednesdays and have 1:1 POCUS workshops in the Simulation center. Each resident will be assigned a POCUS mentor to make sure they stay on track. ▶ Policies
Departmental Policies are detailed here. ▶ Preoperative Services
 Residents complete a two-week rotation at Preoperative Services, a standalone outpatient clinic about 10 minutes from the hospital that has a dedicated on-site attending.
Residents complete a two-week rotation at Preoperative Services, a standalone outpatient clinic about 10 minutes from the hospital that has a dedicated on-site attending.For more information see the General Division. ▶ Program Reviews
Doximity Residency Navigator ranks the Stony Brook Anesthesiology Residency Program #1 on Long Island.
Doximity reviews:
▶ Program’s Overall Competency-Based Goals and Objectives
Stony Brook Anesthesiology Residency Program: Overall Goals and Objectives
The Anesthesiology Residency program has the primary goal of teaching and educating residents to become independent practitioners in the field of anesthesiology by providing a competency - based graded and progressive clinical responsibility experience, teaching the basic components of research and exposing them to the practices of medical education and physician wellness. This goal is attained through an extensive exposure to a diverse population of patients with different degrees of complexity and pathologies in our hospital setting, a strong didactic curriculum and conferences, simulation training, and creating a culture of inquiry through the teaching of skills to develop scholarly activity, quality improvement and patient safety. The Anesthesiology Residency training will take place in an atmosphere of mutual respect and consideration, promoting the ability of residents to acquire the knowledge, skills, clinical judgment and experience that will enable them to independently practice as an Anesthesiologist in a safe and compassionate manner. At the end of the Anesthesiology Residency program, residents are expected to: Patient Care
▶ Regional Anesthesiology Jeopardy Competition
 Congratulations to CA3s Dr. Justin Bell and Dr. Adam Bindelglass for winning the 2024 Anesthesiology Residency Jeopardy Competition in NYC on December 2, 2024! The competition was hosted by the New York Academy of Medicine and several residency programs from NYC and the surrounding area participated.
Congratulations to CA3s Dr. Justin Bell and Dr. Adam Bindelglass for winning the 2024 Anesthesiology Residency Jeopardy Competition in NYC on December 2, 2024! The competition was hosted by the New York Academy of Medicine and several residency programs from NYC and the surrounding area participated. ▶ Research: Clinical, Quality Improvement, and Basic Science
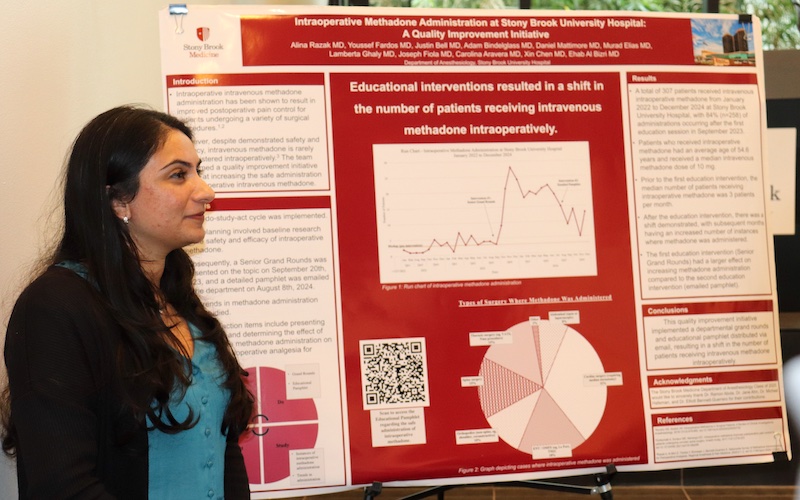
 The Department of Anesthesiology has outstanding infrastructure and opportunities for residents who wish to learn how to conduct clinical research, QA/QI projects and basic research.
The Department of Anesthesiology has outstanding infrastructure and opportunities for residents who wish to learn how to conduct clinical research, QA/QI projects and basic research. Clinical Research We have excellent mentors who have a track record of assisting trainees to design, complete, and publish innovative projects. For example, the Chair (Dr. Bergese) and Vice- Chair for Clinical Research (Dr. Bennett-Guerrero) have both mentored countless individuals over the last 25 years. In addition to expert mentoring, there is dedicated departmental infrastructure to support research including clinical research coordinators, data management and biostatistical expertise, and clinical research space with patient stretcher, monitoring, IV infusion pump, -80 and -30 freezers, refrigerator, and refrigerated centrifuge. The department also offers seed money for promising projects and dedicated research time during the CA-3 year. 
The department is also extremely active in quality improvement projects, especially Enhanced Recovery After Surgery (ERAS). Our former Chairman (Dr. TJ Gan) was the founding President of the American Society of Advanced Recovery (ASER) and is an internationally recognized expert in enhanced recovery. We have a dedicated ERAS coordinator who has been helping us expand from 4 to approximately 10 active protocols in different surgical procedures. Residents are encouraged to be involved in these efforts and are required to complete a QI or patient safety project during residency. Basic Science 
Research Projects Publications ▶ Resident Awards
▶ Resident Call Rooms
 There are 3 call rooms for the 3 on-call main OR residents each night and 1 call room for the OB anesthesia resident on-call. Two of the main OR call rooms are pictured and are well-equipped with a flat screen TV, computer and printer. These two rooms have 2 twin beds and one of the rooms also has a small couch; the third call room for the main OR has one twin bed.  ▶ Resident Presentations at National Meetings
We encourage our Residents to present research posters and Medically Challenging Cases at national meetings such as the ASA and PGA. Residents whose abstracts are accepted for presentation are fully funded to attend the meeting. A listing of the publications and presentations of each resident can be found on the Residents web page. Browse the archives of presentations since 2009. 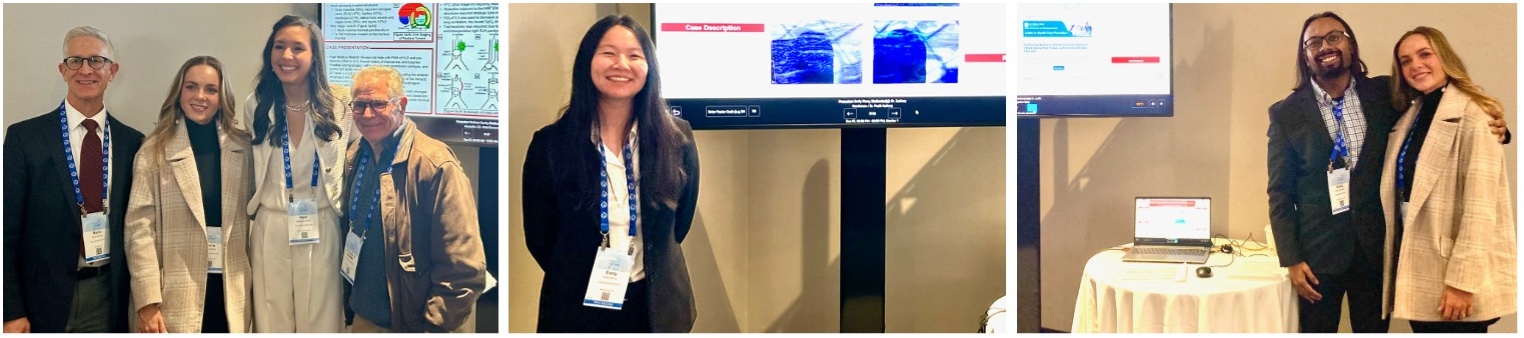
Presentation at NYSSA-PGA 2024
Garrity M, Bodily S, Oleszak S, Boorin M, Epstein R. Anesthetic management of invasive papillary thyroid carcinoma complicated by five tracheal ring resection, tracheal reconstruction, and tracheostomy
Raventhiranathan N, Oleszak S. Jet Ventilation and Airway Management for Patient with Idiopathic Subglottic Stenosis Rahman S, Choudhury N, Bodily S, Oleszak S. Successful Airway Management with Combined Use of Videolaryngoscope and Fiberoptic Bronchoscope in a Patient undergoing Radical Neck Dissection, Total Thyroidectomy and Tracheostomy Wang A, Torpey A, Oleszak S. Anesthetic Management of a Patient with Limb-Girdle Muscular Dystrophy Undergoing an Upper Endoscopy Exam Under General Anesthesia Tsivitis A, Atkinson D, Nguyen N, Feit A. Urgent laparotomy and salpingectomy secondary to ectopic pregnancy in a patient requiring VA ECMO after V fib arrest at home Henein J, Mattimore D, Price J, Zaidi S. A Case of Suspected Fulminant Viral Myocarditis Complicated by Intracardiac Thrombi Starr E, Xiao J, Garrity M, Mays T, Epstein R, Boorin M. Airway Management for a patient with Pierre-Robin Sequence undergoing Dental Rehabilitation Under General Anesthesia Espeleta J, Bargnes V, Fischl A. Don’t Be Conned by Primary Hyperaldosteronism: Anesthetic Considerations for Conn Syndrome DiMaria S, Li J, Cuenca J, Fischl A. Management Of Acute Cardiogenic Shock Secondary To Viral Myocarditis Using Mechanical Circulatory Support Davidson S, DiMaria S, Bargnes V, Feit A, Poppers J. VV ECMO to the Rescue: Successful Recovery from Refractory Intraoperative Anaphylaxis Following Redo Sternotomy for Mitral Valve Replacement Razak A, Ma S, Jin Z, DeLemos M, Bergese SD. Utility of Remimazolam Versus Propofol for Total Intravenous Anesthesia: A Meta-analysis Elias M, Wang E, Hum B, Scott B, Nada E. Regional Anesthetic Approach to Subcutaneous Implantable Cardioverter Defibrillator Placement Nguyen N, Bargnes V, Daoud B, Angelo T, Factor M. Angular pregnancy, Asthma, and Apfel: A Triple-A in Obstetric Anesthesiology: Anesthetic Management of a Patient with Angular Pregnancy Rahman S, Bhimavarapu A, Desai A. Management of Chronic Pain associated with Small Fiber Neuropathy Secondary to SARS-CoV-2 Patel D, Bindelglass A, Wang M. Pre-operative evaluation of a patient with severe glottic stenosis Greenberg S, Bargnes V, Kerolus K, Nada E, Andraous W. Vanishing Phantom Limb Pain Following Adductor Canal and Sciatic Nerve Block with Peripheral Nerve Catheter Infusion Nguyen N, Ahn J, Angelo T, Daoud B, Factor M. Anesthetic Management of a Parturient with Congenital Long QT Syndrome Yerramalli G, Bargnes V, Oster J, Atkinson D, Poppers J. Patient with Heparin-Induced Thrombocytopenia having Adverse Reactions to Heparin having Mitral Clip Placement for Severe Mitral Regurgitation Fiola J, Park G, Price J, Izrailtyan I. Operative Management in Setting of Anomalous Origin of Coronary Artery Shibly Y, Bargnes V, Tannous H, Izrailtyan I. An Urgent CABG Complicated by Coronary Artery Intramural Hematoma from Percutaneous Intervention with Corresponding Electrocardiogram and Echocardiogram Changes in the Setting of Renal Transplantation Monanian G, Factor M, Daoud B, Angelo T. Intraoperative Management of Complete Placenta Previa with Placenta Accreta complicated by Suspected Amniotic Fluid Embolism Lin K, Bargnes V, Bodily S, Elias M, Epstein R, Zabirowicz E. Topicalization & TIVA: A Successful Anesthetic Duo for Endobronchial Oxidized Cellulose Placement in the Treatment of Bronchopleural Fistula Presentation at ASRA Fall 2024
Mangano N. Regional Anesthetic Management of Clavicular and Rib Fractures in an Elderly Patient with Continuous Erector Spinae Block
Presentations at the ASA Meeting 2024
Razak A, Al-Bizri E, Fardos Y, Romeiser J, Bennett-Guerrero E. A Nationwide Survey of Intraoperative Methadone Use for Perioperative Analgesia
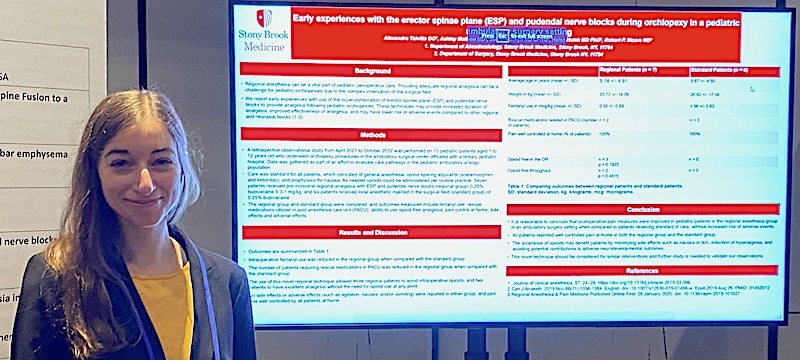
Tsivitis A, Mathew A, Singh S, Hseih H, Moore R. Early experiences with the erector spinae plane (ESP) and pudendal nerve blocks during orchiopexy in a pediatric ambulatory surgery setting Greenberg S, Stephen SR, Abola R, Costa A. Outcomes after Thrombectomy and Thrombolysis for Cerebral Infarction of Various Vascular Territories Murphy J, Chen R, Li D, Kim C, Razak A, Nada E. Trends in Regional Anesthesia Clinical Trials: A Quantitative Analysis of Trials Registered with Clinicaltrials.gov Razak A, Ma S, Jin Z, DeLemos M, Bergese S. Utility of Remimazolam Versus Propofol for Total Intravenous Anesthesia: A Meta-analysis Bargnes V, DiMaria S, Cuenca J, Yammine M, Poppers J. Triple Valve Cardiac Surgery with Bovine Aortic Valve Replacement, Maze Procedure, and Left Atrial Appendage Clipping in a Patient with Alpha-Gal Syndrome Rahman S, Bhimavarapu A, Desai A. Management of Chronic Pain associated with Small Fiber Neuropathy Secondary to SARS-CoV-2 Tsivitis A, Gao M, Caballero J. Combined General and Neuraxial Anesthetic Management with Dexmedetomidine and Bupivacaine in a patient with large bilateral apical bullae undergoing Emergency Exploratory Laparotomy for Small Bowel Obstruction Wang A, Al-Bizri E. External Oblique Intercostal (EOI) Block for Patients Undergoing Nephrectomy for Postoperative Pain Management: A Case Series Oliver B, Bargnes V, Jacob S, Torres G, Marghoob S. Out of My Way! Airway Management of a Patient Presenting for Direct Microsuspension Laryngoscopy and Biopsy with an Obstructing Tonsillar Mass Krauss B, Crugnola WM, Ahn JY, Al-Bizri E. Pre- and Intraoperative Management of Immune Thrombocytopenia and Stroke Risk in a Patient Undergoing Splenectomy Monanian G, Daoud B, Angelo T, Factor M. Management of Congenital Heart Disease and Valvulopathy in a Parturient Torpey A, Vuong W. Anesthetic Management of Patient with OSA and Recent Pneumonia for an Awake Craniotomy for Glioma Resection Bargnes V, Lee E, Oliver B, Razak A, Mathew A, Oleszak S. Perioperative Management of a 25-week Gravid Mother Undergoing Repeat Subglottic Stenosis Dilation Complicated by Tension Pneumothorax and Diffuse Thromboembolic Strokes Monanian G, Elias M, Oleszak S. Management of Airway Complications in the Prone Position Utilizing Fiberoptic and Video Laryngoscope Evaluation Kerolus K, Jacob S, Davidson S, Oleszak S. Considerations for Airway Management for Moebius Syndrome Wang A, Torpey A, Oleszak S .Anesthetic Management of a Patient with Limb Girdle Muscular Dystrophy Receiving an Upper Endoscopy Exam Bargnes V, Chen X, Lin T, Barsch M, Feit A. Cardiogenic Shock Due to Influenza Myocarditis Requiring Extracorporeal Membrane Oxygenation with Complete Recovery of Cardiac Function Greenspan S, Gordon J, Oo J, Caldwell W. Combined Basivertebral Nerve Ablation and Interspinous Spacer Implants Provides Effective Long-term Pain Relief in a Patient with Severe Low Back and Leg Pain Tateosian V, Christophides A, Elias M. Anesthetic considerations of an atypical presentation of a child with Congenital Diaphragmatic Hernia Bargnes V, Ghaly L, Belford J, Aminov J, Oleszak S. Opportune Perioperative Management of a Patient with Multiple Allergies Raventhiranathan N, Oleszak S. Jet Ventilation and Airway Management for Patient with Idiopathic Subglottic Stenosis Andraous W, Kerolus K, Nada E, Bargnes V. Resolution of residual neuropathic limb pain after peripheral nerve block in a patient with below knee amputation Jacob S, Kogan A, Parikh S, Saunders T. Pneumomediastinum Unveiled: An Unusual Finding Post Lumbar Epidural Placement Monanian G, Lee C, Daoud B, Angelo T, Factor M. Intraoperative Management of Complete Placenta Previa with Placenta Accreta complicated by Suspected Amniotic Fluid Embolism Bargnes V, Yonel B, Mangano N, Bitonti N, Wang M, Al-Bizri E. A Bad Headache: Perioperative Considerations for Pediatric Pheochromocytoma Patel D, Bindelglass A, Wang M. Pre-operative evaluation and planning for a patient with severe glottic stenosis Mangano N, De La Hoz M, Oo J, Caldwell W. Basivertebral Nerve Ablation and Spinal Cord Stimulation for Successful Management of Lower Back and Radicular Leg Pain Refractory to Spinal Fusion Surgery Tsivitis A, Jackson L, Al-Bizri E. Successful fiberoptic intubation while maintaining spontaneous ventilation in 6 week old patient with Pierre Robin Sequence Presentations at the American Society of Regional Anesthesia and Pain Medicine meeting Spring 2024
Razak A, Kerolus K, Aravera C, Liu SM, Wang M, Nada E. The Utility of Epidural Analgesia for Acetabular Fractures in Trauma Patients: A Case Report
Razak A, Wozniak S, Nada E. Retroclavicular Approach to the Infraclavicular Region Nerve Block in a Patient with an Upper Extremity Burn Injury Presentation at the Society of Cardiovascular Anesthesiologists 2024
Mattimore D, Chen S, Ahn J, Price J, Poppers J. Delayed Coronary Obstruction Presenting as Myocardial Infarction 5 Years After Transcatheter Aortic Valve Replacement
Presentations at the SOAP Annual Meeting 2024
Lee C, Zhang K, Daoud B, Angelo T, Factor M. Anesthetic Management of Parturient with Severe Mitral Stenosis and Recent Flash Pulmonary Edema
Aravera C, Angelo T, Daoud B, Factor M. Parturient with Klippel Trenaunay syndrome Marzolini L, Zhang K, Daoud B, Angelo T, Factor M. Anesthetic Management of a Parturient with Alpha-Gal Syndrome Nguyen N, Ahn J, Daoud B, Angelo T, Factor M. Anesthetic Management of a Parturient with Congenital Long QT Syndrome Sabetta G, Zhang K, Fardos Y, Mattimore D, Factor M. A Case of Pancytopenia in a Parturient with Autoimmune Hepatitis undergoing Cesarean Section Presentations at the Soc Ped Anes 2024
Tsivitis A, Kozlowski P, Corrado T, Chesler D, Moore R, Al-Bizri E. Traumatic carotid artery injury caused by a metal sipping straw in a pediatric patient: Anesthetic management and considerations
Tsivitis A, Mathew A, Singh S, Hsieh H, Moore RP. Early experiences with the erector spinae plane (ESP) and pudendal nerve blocks during orchiopexy in a pediatric ambulatory surgery setting Presentations at the Am Soc Dental Anes 2024
Xiao J, Raventhiranathan N, Epstein R, Boorin M, Oleszak S. Jet Ventilation for Subglottic Stenosis: Case Report and Algorithm for Diagnosis and Treatment of Pneumothorax
Frusetta C, Bodily S, Epstein R, Boorin M, Oleszak S. An Unanticipated Oxygen Desaturation following Emergence from a Routine General Anesthetic Presentations at the PGA December 2023
Rakhamimova E, Jin Z, Lin J. Comparison of liposomal bupivacaine to conventional local anesthetics in adductor canal block for knee surgery, a meta-analysis
Murphy J, Razak A, Jin Z, Wang M. Efficacy Of Liposomal Bupivacaine Versus Local Anesthetics In Transversus Abdominis Plane Blocks: A Meta-analysis Aravera C, Angelo TE. The Lasting Effects of COVID on a Parturient Requiring ECMO for Cesarean Delivery Richman DC, Jin Z. You Did What!? You Placed a Drug Eluting Stent Prior to This Time Sensitive Surgery!? And It Is Safe to Hold Clopidogrel at 30 Days? Muncan B, Bell J, Daoud B, Elias M, Factor M, Angelo T. Neuraxial Anesthesia in an Obstetric Patient with Transverse Myelitis Garry E, Elias M, Angelo T, Daoud B, Factor M. Anesthetic Considerations for a Parturient with Congenital Long QT Syndrome and an Implantable Cardioverter-defibrillator Rakhamimova E, Elias M, Angelo T, Factor M. Anesthetic Management of a Parturient with a Symptomatic Pericardial Effusion. Bargnes V, Fiola S, Nguyen V. Patient with Alpha-Gal Syndrome Is Allergic to Heparin Having Living Donor Renal Transplant Shibly Y, Hum B, Lee C, Zhang K. Anesthetic Management and Considerations for Transcarotid TAVR Rupert D, Fardos Y, Parikh S, Oleszak S. Intraoperative pulseless electrical arrest, Pneumomediastinum, and Bilateral pneumothorax at time of emergence after total thyroidectomy Hum B, Fischl A, Lee C, Shibly Y, Zhang K. Management of Severe Pulmonary Hypertension During Open Inguinal Hernia Repair Under Epidural Chernoff D, Jin Z, Tsivitis A, Al-Bizri E. Single Shot Fascia Iliaca Plane Block for Femur Fracture in a Pediatric Trauma Patient Oliver B, Jacob S, Winter G, Epstein R, Oleszak SP. Airway Management of an Adult Patient with Pierre-Robin Sequence Presenting for Closure of Gastro-cutaneous Fistula Ghaly L, Zimmerman A. Use of Stellate Ganglion Block for Post COVID-19 Pleuritic Chest Pain Curran L, Kim EK, Richman D. The Thirteenth Lead on the Twelve Lead ECG Curran L, Kim EK, Richman D. Between a Stone and a Hard Place Presentations at the American Society of Regional Anesthesia and Pain Medicine Annual Meeting Fall 2023
Rahman S, Desai A, Moore R. Erector spinae plane block for cancer related brachial plexus pain - A new role for regional anesthesia in NORA?
Ghaly L, Zimmerman A, Kaushal A. The use of stellate ganglion block for post- covid-19 pleuritic chest pain. Presentations at the ASA Meeting 2023
Razak A, Murphy J, Jin Z, Wang M. Efficacy of Liposomal Bupivacaine Versus Local Anesthetics in Transversus Abdominis Plane Blocks: A Meta-analysis
Lin J, Mousumi M, Mukherjee M, Jin Z, Li R. Systemic Review and Meta-analysis of Postoperative Inflammatory Cytokines in Cancer Surgery Under Inhaled or Intravenous Anesthetics Rupert D, Wang K, Hafeman M, Lai L, Schabel JE. Publication Rates and Time to Publication for American Society of Anesthesiologists: A Retrospective Analysis Lin J, Jin Z, Mousumi B, Mukherjee MB, Li R. The Potential Role of General Anesthetics in Cancer Surgery: Meta-analysis of Postoperative Metastasis Ghaly L, Oleszak SP. Use of Combined Video and Fiberoptic Laryngoscopy for Conversion from Oral to Nasal Intubation in an Anticipated Difficult Airway Jacob S, Bell J, Pyo R, Izrailtyan I. TandemHeart for High Risk PCI with LV Thrombus Elias M, Zhu M, Liu SM. Management of a Difficult Airway in a Patient with Advanced Head and Neck Sarcoma Bargnes V, Rakhamimova E, Angelo TE, Factor M, Schabel JE, Daoud BE. Peripartum Management of a Patient with May-Hegglin Anomaly Bargnes V, Rismany J, Schabel JE, Factor M. Peripartum Management of a Parturient with Acute Fatty Liver of Pregnancy and Twin Gestation Razak A, Urquart D, Winter G, Aravera C, Oleszak SP. Airway Management Strategies for a Patient with a Large Hypopharyngeal Mass with Effacement of the Supraglottic Airway Elias M, Patel A. Perioperative Management of a Patient with Alpha-Gal Allergy Undergoing Emergency Surgery Chen X, Raj A, Oleszak SP, Wang M. Stridor and Cervical Fracture: Worst Combination in Airway Management Hum B, Lee C, Zhang K, Hafeman M, Atkinson DJ. Management of Cardiac Tamponade Following Incidental Puncture of Pericardium During Mechanical Thrombectomy Raj A, Fiola JD, Mena S, Oleszak SP. Successful Nasal Fiberoptic Intubation in a Patient with an Expanding Lingual hematoma, Extensive Oropharyngeal Injury, and Bleeding From the Upper Airway as a Result of a Penetrating Gunshot Wound Angelo T, Aravera C, Daoud BE, Factor M. Severe Long Term Sequela of COVID-19 requiring ECMO for CD Fardos Y, Elias M, Beg T, Poppers JS. Diagnosis and Management of Intraoperative PE during Orthopedic surgery requiring ECMO Shibly Y, Ahn J, Factor MG, Angelo TE, Daoud BE. Management of a Parturient with Severe Mitral Stenosis Ghaly L, Oleszak SP, Fleischer LH. Management of a Patient with Multiple Allergies to Anesthetic Medications Kim E, Elias M, Atkinson DJ, Poppers JS. Perioperative Management of a Patient with C1-esterase Inhibitor Deficiency Undergoing Cardiac Surgery Gombert A, Fardos Y, Daoud B, Factor M, Angelo TE. Obstetric Anesthetic Considerations and Management in a Patient with Pompe Disease Elias M, Kim EK, Zabirowicz E. Perioperative Management of a Patient with Factor VII Deficiency Undergoing Cardiac Surgery Bell J, Azim SA. Post Operative Vision Loss in a Twelve Year Old Following Spine Surgery Tsivitis A, Chernoff D, Jin Z, Al Bizri E. Pediatric Regional Anesthetic Management of Femur Fracture with Single Shot Fascia Iliaca Plane Block Bargnes V, Rahman S, Lehman FR. Massive Aspiration Event in the Setting of Undiagnosed Multiple Sclerosis Gastroparesis Presentations at the International Anesthesia Research Society Meeting 2023
Jin Z, Kowa C, Hum B, Bennici L, Liu S. Pericapsular Nerve Group Block versus Fascia Iliaca Block for Postoperative Analgesia after Hip Surgeries, a meta-analysis .
Jin Z, Rakhamimova E, Lin J, Nada E. Comparison of liposomal bupivacaine to conventional local anesthetics in adductor canal block for knee surgery, a meta-analysis. Presentations at the SOAP Annual Meeting 2023
Zhang K, Daoud BE, Angelo TE, Factor M. Anesthetic Management of a Parturient with a Mediastinal Tumor after Intrapartum Chemotherapy.
Lee C, Daoud BE, Angelo TE, Factor M. Anesthetic Management of the Parturient with Chronic Myeloid Leukemia and Associated Splenomegaly. Aravera C, Angelo TE, Factor M, Daoud BE. Anesthetic Management of a Parturient with Post-COVID ILD, Large Pulmonary Bulla, and Acute-on-Chronic Respiratory Failure. Hum B, Shafai A, Angelo TE, Factor M, Shibly Y, Daoud BE. Management of a Parturient with Aortic Stenosis and Worsening Aortic Coarctation. Shibly Y, Shafai A, Angelo TE, Factor M, Hum B, Daoud BE. Management of a Parturient with ESRD and Worsening Pericardial Effusion. ▶ Residency Program Leadership
▶ Resident Research Track
The Stony Brook Mentored Anesthesiology Research Track (SMART) is a highly selective residency track designed to increase the number of graduates pursuing academic careers by offering trainees dedicated research experience while meeting the American Board of Anesthesiology (ABA) clinical training requirements for residency. Selected residents will receive additional research training and mentoring as they prepare to become future physician scientists. The resident research track option in anesthesiology residency is recognized by the Accreditation Council for Graduate Medical Education (ACGME) and the American Board of Anesthesiology (ABA). ▶ Resident Life
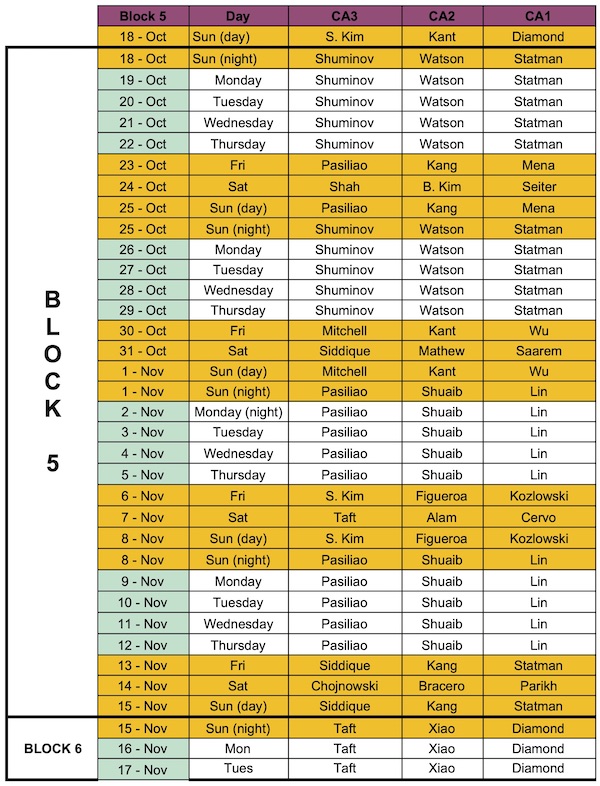
Rotations at Stony Brook Medicine assigned as four-week blocks
Resident Wellness
 Meet our current residents. How we have fun! Our resident Instagram page ▶ "Resilience at the Brook" Respite Room
Stony Brook University Hospital has an onsite a respite room that is open 24/7 for residents and staff. It has a massage/vibration chair, yoga mats, color-by-number books and pencils, comfy couches, TV and tables to eat at. It’s a great place to take a break.
 ▶ Rotation Experience
A day-in-the-life of a Resident on Rotation
▶ Salary and Benefits
The residents in the Department of Anesthesiology receive a salary that fits in the highest range in the country. The salary base is contractually increased annually. Full malpractice coverage of all clinical activity performed in the course of duty, basic and major medical insurance, dental insurance and a drug prescription plan are provided. Residents receive four weeks vacation leave per annum. Residents have the opportunity to attend a major national Anesthesiology meeting every year.
Current salary information Telephone information: 631-632-6770 House Staff Office: 631-444-2754. ▶ Sample Resident Main OR Weekend Call and Night Float Schedule
▶ Teaching Hospitals
Resident training in Anesthesiology is provided in two medical centers: Stony Brook University Medical Center and the Northport Veterans Administration Hospital.
 Since we began providing care in 1980, the staff of Stony Brook University Medical Center has been committed to delivering excellence in patient care, research, education, and community service. Since we began providing care in 1980, the staff of Stony Brook University Medical Center has been committed to delivering excellence in patient care, research, education, and community service.
 Northport Veterans Administration Medical Center offers quality medical, surgical, psychiatric, rehabilitative and skilled nursing care to Long Island veterans. With highly qualified and experienced healthcare professionals, state-of-the-art technology, a full range of services, and high ratings with the Joint Commission on Accreditation of Healthcare Organizations and other respected accrediting health care organizations, Northport VA Medical Center has a reputation for providing superior healthcare to Long Island's veterans. Northport Veterans Administration Medical Center offers quality medical, surgical, psychiatric, rehabilitative and skilled nursing care to Long Island veterans. With highly qualified and experienced healthcare professionals, state-of-the-art technology, a full range of services, and high ratings with the Joint Commission on Accreditation of Healthcare Organizations and other respected accrediting health care organizations, Northport VA Medical Center has a reputation for providing superior healthcare to Long Island's veterans.
▶ Teaching Opportunities
There are plenty of opportunities to teach as a resident. Because anesthesiology is a mandatory 2-week medical student rotation at Stony Brook, we have 140 students rotating through the OR each year to learn clinical anesthesia and often an additional 15- 25 elective medical students. The medical students are paired to work with residents, and residents typically enjoy having an opportunity to teach students during their clinical day. We also have a variety of other learners that are paired with the residents in the main OR for their anesthesia experience. They include dental residents, periodontal residents, dental students, EM residents, ENT residents, neurosurgery residents, and orthopedic surgery residents.
One Chief Resident per year serves as the “Chief Resident for Medical Student Education.“ This Chief assigns the students to specific ORs each day to assist the students with meeting their goals and objectives for the rotation. Senior residents have an opportunity to teach junior residents when on call and on OB. In our program, the CA3s act as a junior attendings when on call to learn how to triage cases and assist with the supervision of the CA1s and CA2s for induction, emergence and intraoperative care. Regarding classroom teaching, our department gives 12-18 medical student lectures each month. Residents can volunteer to teach some of these lectures if they like. All of our Education Day resident lectures are given by faculty, but residents have an opportunity to teach their peers and faculty during Journal Club presentations, QA grand rounds and their senior presentations. 
Dr. Adam Bindelglass the 2025 Resident Teacher of the Year. In sum, there are many opportunities to teach and you be rewarded for doing a good job. 😊 ▶ Teaching Videos
▶ Testimonials
Alina Razak, MD 2025 Resident Graduate, Stony Brook Department of Anesthesiology 2025-26 Regional Anesthesia Fellowship, Johns Hopkins 
Clinically, the training is exceptional. We manage a wide range of complex cases, including high-acuity obstetrics, trauma, and medically challenging surgical patients. The diversity of our case mix—from general surgery and orthopedics to thoracic surgery and acute pain—has prepared me to feel confident in any clinical setting. Each rotation pushed me to grow, and I always felt supported by my mentors and peers along the way. Another strength of the program is the professional network we build through our faculty. Thanks to their connections, I was able to secure a job in the South that aligned perfectly with my career goals. I leave this program not only with strong clinical skills, but with lifelong colleagues, mentors, and friends. I’m proud to be a graduate of Stony Brook Anesthesiology and feel fully prepared to take the next step in my career with confidence and independence." Murad Elias, MD 2025 Resident Graduate, Stony Brook Department of Anesthesiology Present: Private practice in South Carolina 
The clinical training was rigorous and well-rounded. I had the opportunity to manage complex cases across multiple subspecialties and sharpen my procedural skills in high-acuity situations. The attendings challenged me to think critically while remaining approachable and deeply invested in my growth. By my final year, I was trusted with the autonomy to function at the level of a junior attending. I leave this program confident in my abilities and well-prepared to face the challenges of independent practice. Beyond the clinical experience, what really stood out to me was the culture. Residency was intense, but what made the difference here was the sense of community. I had the chance to form genuine friendships with attendings and co-residents, and those relationships helped carry me through the tough moments. I always felt like I had people in my corner. As I graduate and step into attending life, I know that Stony Brook gave me the tools I need—not just to succeed, but to thrive and lead with integrity and compassion. I’m proud to have trained here, and I’ll always carry the lessons and values I gained with me." Youssef Fardos, MD 2025 Resident Graduate, Stony Brook Department of Anesthesiology Present: Private practice 
Daniel Mattimore, MD 2025 Resident Graduate, Stony Brook Department of Anesthesiology 2025-26 Cardiac Anesthesiology Fellowship, Duke University Medical Center 
By the time I graduated, I felt well equipped with both the technical skills and clinical knowledge required for a new grad who was about to start practicing independently. My training at Stony Brook provided a solid foundation, enabling me to confidently fulfill my responsibilities as an attending anesthesiologist at a tertiary care hospital with Level 1 trauma and a busy Labor & Delivery, where I supervise residents and CRNAs. I am grateful for the opportunities that shaped me into the anesthesiologist I am today and am thankful to everyone who helped me along the way. The residency program here is simply outstanding and provides the highest level of training." Shruti Parikh, MD 2023 Resident Graduate, Stony Brook Department of Anesthesiology Present, Anesthesia Attending, Stony Brook Department of Anesthesiology 
I had always heard that the learning curve from medical student to anesthesia resident was steep. The early months as a CA-1 were exciting, yet exhausting having to learn practical aspects of anesthesia in the operating room, and then going home and burying my face in books and question banks to help bring concepts together. I have never been a good test taker and had an immense weight on my shoulders to pass the Basic Exam after not performing well on the yearly Inservice Training Exam. With tremendous support from our program directors, faculty mentors, and department as a whole, I had every resource available to study and prepare for this daunting exam which resulted in me passing on the first attempt. This was a huge milestone for me as someone who has always let nerves and second-guessing get the best of me on test day. During my CA-2 year, I made the decision to pursue a fellowship in one of the most challenging subspecialties: Adult Cardiothoracic Anesthesiology, fully knowing that I was not a competitive applicant. I saw the fellowship as an opportunity to sharpen my skills as an anesthesiologist, while also adding powerful new tools like mastery of the pulmonary artery catheter and transesophageal echocardiography to my clinical repertoire. I am confident in saying that I would not have made this decision in my career without my incredible attending mentors here at Stony Brook. Starting CA-3 year brought on a new challenge as I took on the task of learning the role of an attending. I now found myself in the position of deciding and acting upon my own anesthetic plans, teaching and supervising junior residents (surprisingly more challenging than I expected), performing echocardiography, and many other tasks. As the year progressed, attendings granted me more autonomy, letting me start and perform cases on my own, and acting as the attending for junior residents. I continued to hone my technical skills and grow my confidence in mechanical skills I once found daunting from arterial lines and central lines to peripheral nerve blocks, all knowing that in just a few short months I would be the one helping, teaching, and supervising others in those same tasks. And again, for this, I have immense gratitude for my training. Aside from the excellent clinical training, perhaps one of the most irreplaceable things completing a residency at Stony Brook has given me is lifelong friends. I know it may sound cliche, but I was very lucky to have trained alongside a group of like-minded individuals with common interests who formed a bond that will be hard to break. If I had to do residency all over again, as a soon-to-be cardiac anesthesiologist, I would choose Stony Brook in a heartbeat!" Victoria Nguyen, MD 2024 Resident Graduate, Stony Brook Department of Anesthesiology 2024-25 Fellowship, Cardiothoracic Anesthesia, University of Pittsburgh 
Michael Hafeman, MD 2024 Resident Graduate, Stony Brook Department of Anesthesiology 2024-25 Pediatric Anesthesia Fellowship, Laurie Children’s / Northwestern University 
I applied for anesthesiology residency in a unique situation – couples matching with my significant other who was also applying for anesthesiology. We interviewed at programs across the country and encountered many skeptics, people who saw our relationship as a liability rather than an asset. Stony Brook was not one of them. The faculty at Stony Brook welcomed me and Chris (who is, spoiler alert, now my coresident) with open arms from day one and that support has not once wavered or been challenged. And now as I sit here one month from graduating, I cannot imagine having done my training anywhere else. I will forever be grateful to the institution that saw me as more than a statistic and gave me the chance to go through residency with my best friend. The Stony Brook anesthesiology department has become my second family, and I have no doubt that the relationships I’ve formed will continue on well after I’ve graduated." Kalissa Zhang, MD 2024 Resident Graduate, Stony Brook Department of Anesthesiology 2024- Private Practice, California 
I would describe our training as both robust and eclectic, with a strong case mix Index, as documented by CMS. We are exposed to a wide array of cases, and residents have an appropriate amount of supervision at first, which matures into more autonomy as we grow our clinical skills. As a CA-1, we get our reps in on general cases, but as a CA-3 resident, we function as junior attendings. Helping to manage the OR Front Board and build the daily OR schedule while simultaneously developing our anesthetic plans and delivering them in the OR. Our clinical skills are cultivated by a robust educational program, which our faculty lead. Every month we as a class are excused from clinical responsibilities to attend simulation sessions and lectures, in which the department caters food for lunch and faculty members discuss keywords and topics pertinent to our board exams and future practice. Above all the amazing clinical and educational experiences Stony Brook offers, I also value the personal relationship I have developed with my classmates, faculty, and residents from within the department and from various other specialties in the Hospital. Weekly meet-ups with classmates, snowboarding trips, academic conferences, and even summer getaways to Fire Island are memories I will never forget. All in all, I had an amazing experience at Stony Brook. The program has only elevated my clinical and academic skills, making me the physician I am today." Giacomo Scorsese, DO 2023 Resident Graduate, Stony Brook Department of Anesthesiology 2023-24 Cardiac Anesthesiology Fellowship, Mt. Sinai East, New York 
Christopher Seiter, DO 2023 Resident Graduate, Stony Brook Department of Anesthesiology 2023-24 Cardiac Anesthesiology Fellowship, Vanderbilt University 
Aria Shafai, MD 2023 Resident Graduate, Stony Brook Department of Anesthesiology 2023-24 Obstetric Anesthesiology Fellowship, Columbia Presbyterian 
I left Stony Brook with confidence that the versatile skills that I had learned had given me a solid foundation to tackle any case that I may encounter in my career. Being the largest medical center in the area, Stony Brook, provided me the opportunity to see a wide range of pathology and an unparalleled breadth of cases. Equally important, if not more so, I left Stony Brook still feeling human, I never felt that I was a 'cog in the machine'. It was actually quite the opposite, the priority was to have residents placed in the clinical environments that would have the most teaching potential. In fact, entire days have clinical duties shaved away so that residents could focus on didactics and 'life stuff' which meant I never got a cavity during residency because I always knew when I could schedule a dental appointment. During my final year of residency I ran the recruitment process for incoming applicants and the question that I heard the most was 'How do I go about ranking programs?'. Personally, the program you choose should have an environment or 'feel' that will help you thrive. So the question becomes, what is Stony Brook's 'feel'. The answer: cosy atmosphere at a big institution. " Karim Shuaib, MD 2022 Resident Graduate, Stony Brook Department of Anesthesiology 2022-23 Obstetric Anesthesiology Fellowship, Columbia Presbyterian 
Carlos Figueroa, MD 2022 Resident Graduate, Stony Brook Department of Anesthesiology 2022-23 Pediatric Anesthesiology Fellow, Hofstra 
Ashley Mathew, MD 2022 Resident Graduate, Stony Brook Department of Anesthesiology 2022-23 Pediatric Anesthesiology Fellow, DC Children's 
Ramanjot Kang, MD 2022 Resident Graduate, Stony Brook Department of Anesthesiology 2022-23 Pain Fellow, Cornell 
Ishu Kant, MD 2022 Resident Graduate, Stony Brook Department of Anesthesiology 2022-23 Pain Fellow, Mt. Sinai West 
Lucas Bracero, MD 2022 Resident Graduate, Stony Brook Department of Anesthesiology 2022-23 Chronic Pain Fellow, Cornell University Medical Center 
Duran Ryan Mitchell, MD, MBA 2021 Resident Graduate, Stony Brook Department of Anesthesiology 2021 MBA Graduate, Brandeis University 2021-22 Chronic Pain Fellow, Duke University Department of Anesthesiology 
Josiah Miles, MD, 2021 Resident Graduate, Stony Brook Department of Anesthesiology 2021-22 Cardiac Anesthesiology Fellow, Albert Einstein Medical Center 
"Stony Brook Anesthesia residency is an excellent program with great faculty and amazing co-residents! This program prepares you well to take on the real world, whether it be private or academic practice. Our residents always match well to fellowships in the fields they want and have amazing support from our faculty. We do plenty of complex cases and have the opportunity to do many, many procedures. There are actually no anesthesia subspecialty fellows here, so we work directly with pediatric, cardiac, and pain attendings and get plenty of 1-on-1 teaching. Intern year acclimates you to the system and you work with your future subspecialty colleagues. Other benefits are that we have an academic day every three weeks where we get to come together as a class, enjoy a free meal, and get lectures from our attendings. All of our residents look forward to this day. We also get a generous education stipend which helps pay for our licensing and board exams. They even give us additional education funds if we do well on our in-training exams. Lastly, we have an amazing program director who really goes above and beyond for the residents. She is a true resident advocate who supports us and stands up for us. I think the program is small enough (10 residents per class) that we all get to know each other really well, but it's big enough that we get to do a wide variety of cases. Overall, residency was a great experience, and it has taught me to become a confident anesthesiologist!" After Fellowship "Stony Brook's anesthesia residency program does a great job of preparing you for the next step, whether it is fellowship or private practice. During fellowship, I appreciated how much I got to do during residency at Stony Brook because I was not competing for cases or procedures with fellows. The residents at Stony Brook get to work directly with attendings and learn from them 1 on 1, even in the most complex, high risk cases. I also realized during fellowship that a medium-sized residency program is great because you can actually keep in touch with all of your co-residents after residency and see that everyone is doing well. Stony Brook did an excellent job of preparing me for fellowship" Manuel Lee, MD 2020 Resident Graduate, Stony Brook Department of Anesthesiology Pediatric Anesthesiology Fellow 2021-22 Department of Anesthesiology & Critical Care Medicine Johns Hopkins School of Medicine 
RIchard Tenure, MD 2020 Resident Graduate, Stony Brook Department of Anesthesiology 2020-21 Critical Care Fellow, Hospital of the University of Pennsylvania 2021-22 Cardiac Anesthesia Fellow, Massachusetts General Hospital 
"If I were making my rank list again today, I would 100% without hesitation put Stony Brook as my #1 choice for anesthesia residency. I could not be happier with the training and experience I received. During my tenure there and afterwards, the faculty invested in my education and professional development. It is remarkable what can be achieved with mentors and faculty that invest in you as a physician and adult learner. I was an average medical student at best. The experience, resources, and opportunities at Stony Brook Anesthesia propelled me to one of the most competitive fellowship positions in our field, first author on original research and book chapters, and ready to take on any challenge the day after graduation." After Fellowship "Having completed cardiac fellowship I now see how lucky I was to have done my general anesthesia training at Stony Brook. We got to do all of the most complex cases with attendings who were focusing on getting you as an individual to the next level of practicing anesthesia. Little did I know when I was in residency how well recognized our attendings are on the state and national stage as teachers, clinicians, and researchers. So many times during the last year I remember using things my attendings at SB had taught me to guide me through an acute situation in the OR...and yes, referencing all of Dr. Poppers' handouts. Residency at Stony Brook 100% put me ahead of the curve to start fellowship." Leif Ericksen, MD 2020 Resident Graduate, Stony Brook Department of Anesthesiology 2020-21 Cardiac Anesthesia Fellow, NYU Department of Anesthesiology 
Demetri Adrahtas, MD 2019 Resident Graduate, Stony Brook Department of Anesthesiology 2020 Cardiac Anesthesiology Fellow, Rutgers University 
Michael Khalili, MD 2019 Residency Graduate, Stony Brook University Department of Anesthesiology 2019-2020 Pain Management Fellow, Columbia University Department of Anesthesiology 
Sofia Geralemou, MD Graduate, Stony Brook Residency Program 2011 
"The best way I would describe my experience in anesthesia at Stony Brook is an excellent place for clinical training, with knowledgeable and friendly faculty, and great educational resources. Add to that the location of being in Long Island, with many different active and entertaining venues on its own, not to mention that it's just a train ride away from NYC, being here is the complete package. The department at Stony Brook was recently ranked #6 nationwide in NIH funding to an anesthesia department, and this is the result of the commitment they put into education and research. In fact, I was able to begin my research career here through the 6 month research track they offered during the 3rd year of my anesthesia residency. This research flourished and after receiving grant funding for my work, I decided to continue my research as faculty here at Stony Brook Anesthesiology. I am excited at the direction our department is moving, as we continue to grow and expand, and I look forward to working with each new resident group that joins our department. I certainly found the perfect anesthesia residency match for me and my career, hope you are able to find the same for you. Good luck!" Rany Makaryus, MD Graduate, Stony Brook Residency Program 2010 
I came out of Stony Brook feeling extremely comfortable providing anesthesia for my patients and, quickly, my new practice had confidence in me. I really attribute this to the amount of attention each resident receives at Stony Brook as they do their clinical work. The feedback I received from the residency program allowed me to adjust my skills to make me the safest and most efficient anesthesiologist I could be. And further, the exposure to all anesthesia related procedures is unbeatable by any program in the U.S. in my opinion. I graduated from the program able to easily and quickly insert various central lines, arterial lines, and perform peripheral nerve blocks for regional anesthesia. I came out of Stony Brook highly proficient in regional anesthesia. As an attending for 7 years, I have seen many new graduates incapable at performing regional anesthesia at the level of any graduates of the Stony Brook Anesthesiology Program that have joined my practice after me. As a result of my experience at Stony Brook, I not only passed my boards on the first attempt, I joined the largest physician run anesthesia group in New Jersey, Morris Anesthesia Group. I quickly took on a leadership role and in my first year was promoted to Director of Regional Anesthesia. I truly believe Stony Brook brings something special to the table and that is teaching its residents how to be leaders in the world of anesthesia. Now, 7 years out of residency, I am not only a managing partner of Morris Anesthesia, but I was just named Chief of Anesthesia at our hospital. I attribute this great achievement to the place it all started. The experience that residents get at Stony Brook is priceless and I cherish my decision in listing Stony Brook as my number one choice for anesthesia residency." Jason Daras, DO Graduate, Stony Brook Residency Program 2010 Director of Regional Anesthesia Morris Anesthesia Group, Parsippany, NJ Mark Kim, MD and Jonathan Tan, MD (Graduates, Stony Brook Residency Program 2013) discuss their residency experience at Stony Brook Anesthesiology. ▶ University/Community
Stony Brook University
Stony Brook's reach extends from its 1,100-acre campus on Long Island's North Shore: encompassing the main academic areas, an 8,300-seat stadium & sports complex, a performing arts center, Stony Brook University Medical Center, the Health Sciences Center, and the Veterans Home to Stony Brook Manhattan, a new Research and Development Park, three business incubators and the new Stony Brook Southampton campus on Long Island's East End. Stony Brook also co-manages Brookhaven National Laboratory Stony Brook is still growing. To the students, the scholars, the health professionals, the entrepreneurs, and all the valued members who make up the vibrant Stony Brook community, this is a not only a great local and national university, but one that is making an impact on a global scale. Surrounding Community
Three Village Patch - local activities  ▶ Videos
2018 CA-3 Residents' patient education video about labor epidurals ▶ Visiting Professors
The department sponsors a monthly Visiting Professor lecture series. Invited speakers present clinical and/or research topics at our Wednesday morning Grand Rounds. Whenever possible, the Visiting Professor makes a separate presentation to the Residents on Tuesday afternoon.
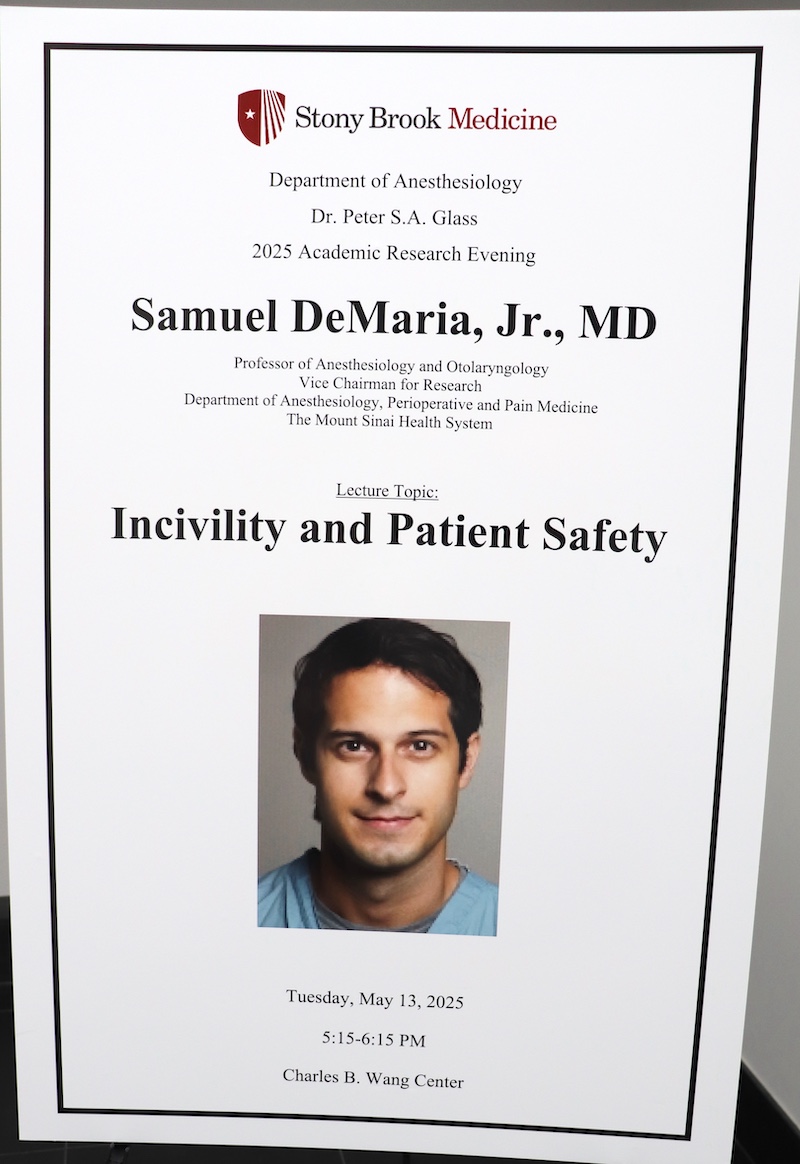
The Visiting Professorship in April or May is combined with our annual Peter S. A. Glass Academic Research Evening. During the poster session, Residents, Faculty and Students present display their research accomplishments. Several Residents and Students are selected to give oral presentations as well. The Visiting Professor presents the keynote speech. This is followed by dinner and an awards ceremony. ▶ Wellness
The Department of Anesthesiology is so committed to the wellness of their residents that it has a dedicated Wellness and Social Chair for the Residency Program! The Wellness Chair selects and coordinates social events for the program and keeps tabs on the overall morale and wellness of the residents. Previous program wellness events have included fishing trips, Spartan Race, BBQs, pool parties, baseball games, skeet shooting, dinners, ski trips, bowling parties, holiday parties, paintball, Halloween parties,… Institutional wellness events have included annual puppy socials, BBQs on the patio, ice cream socials, and wellness fairs. In addition to the departmental and institutional social events, the anesthesiology residents receive 1-2 all-day, nonclinical education days for their class each month. These all-day education days further promote wellness and peer support by regularly bringing each residency class together during scheduled breaks from the hustle and bustle of clinical training.
To learn more about the institution’s commitment to wellness, please visit. https://renaissance.stonybrookmedicine.edu/gme/wellness. A comment from one of the anesthesia residents is highlighted! ▶ Women in Anesthesia Journal Club
The WIA Journal Club brings women in the department together to foster an environment of support and mentorship among attendings and residents.
Dr. Tazeen Beg hosts the meetings at her home. Topics of discussion included women in leadership and potential obstacles that women face. At one meeting, Dr. Beg surprised the group by having an author of one of the articles join the discussion via Zoom.
▶ Youth Outreach
Science and Research Awareness Series (SARAS) is a 3-week, summer program designed to heighten the awareness of High School and Undergraduate students in many aspects of Biomedical Science. The program is sponsored by the Department of Anesthesiology and directed by Dr. Srinivas Pentyala. Many of our faculty members, residents and medical students participate in SARAS lectures and workshops. SARAS has been offered since 2004 and typically attracts over 100 participants, including high school students from backgrounds underrepresented in medicine.
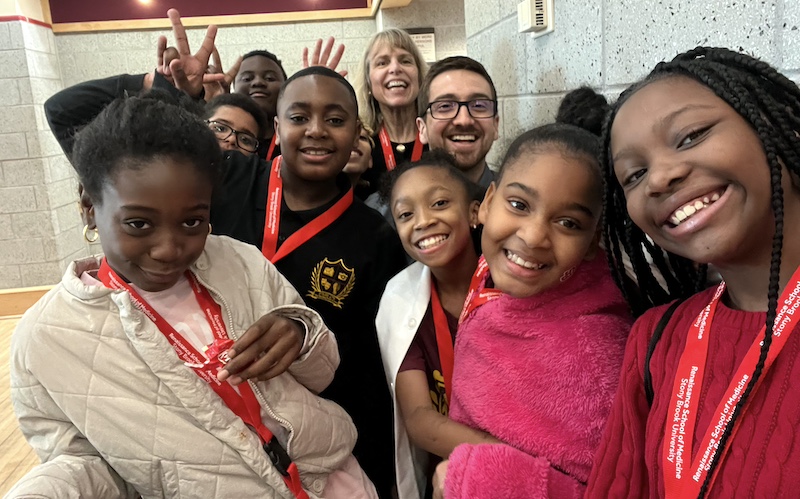
The Department of Anesthesiology and Stony Brook Medical Center partnered with the American Medical Association (AMA) in their shared commitment to dismantling structural racism and increasing diversity in the physician workforce. Members of the Department of Anesthesiology participate in the annual Stony Brook “Black Men in White Coats” Youth Summit. Over 500 youth from backgrounds underrepresented in medicine attend the event. Black Men in White Coats is an AMA-created documentary that inspires to increase the number of Black men in the field of medicine. During the summit, participants examined the structural barriers to increasing diversity in medicine from the perspectives of Black men who are both physicians and leaders in medicine. Photos and videos from the 2024 Summit. 
Left: Resident Dr. Sadiq Rahman with Dr. Getu Teressa, Associate Prof of Clinical Medicine Right: Dr. Rahman with Dr. Schabel 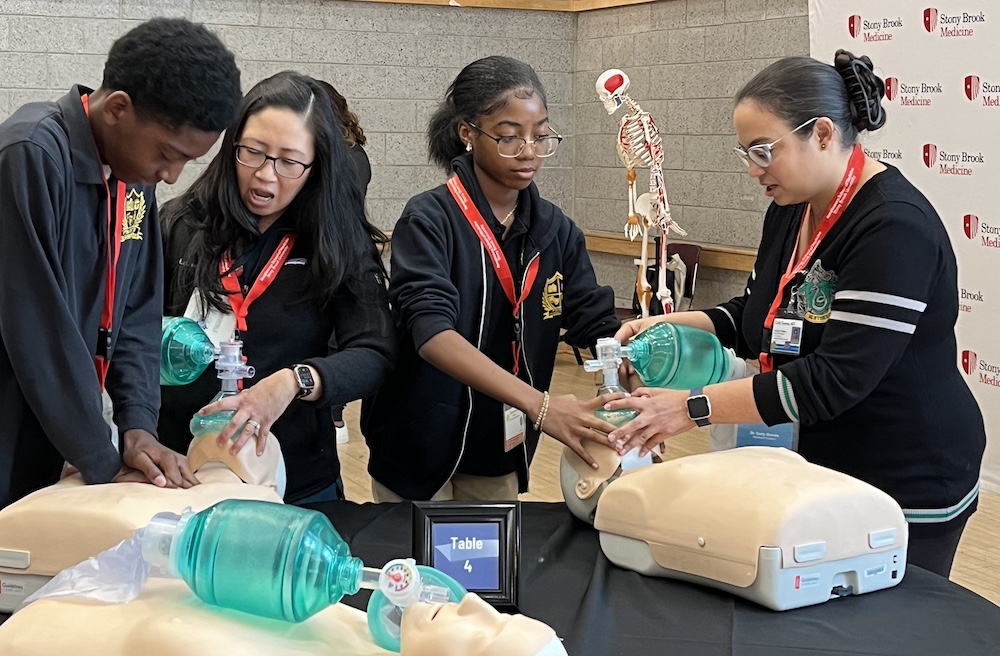
HOPE (Health Occupations Partnership for Excellence) is a joint venture between Stony Brook Medicine and the Brentwood, Longwood, and Wyandanch School Districts. High school juniors and seniors from these districts meet with Stony Brook health care professionals and scientists to learn more about the inner workings of the hospital and the variety of jobs that are involved. The ultimate goal of the program is to increase the number of students from underrepresented and ethnic minority backgrounds who pursue careers in medicine. The current HOPE mentors from the Department of Anesthesiology are Drs. Ana Costa, Tazeen Beg, Stephen Vitkun and Srinivas Pentyala. 
|






 From its beginnings in 1957,
From its beginnings in 1957,  The Stony Brook area is one of the most attractive residential communities in the Northeast. Amid the hilly dunes near Long Island Sound the woods and fields along the water offer a variety of scenic delights. Fishing, boating, golf and horseback riding are among the many opportunities for recreation. Small wonder that the area has always been attractive to artists and scholars. The local museums and neighboring communities provide recreation and educational experience.
The Stony Brook area is one of the most attractive residential communities in the Northeast. Amid the hilly dunes near Long Island Sound the woods and fields along the water offer a variety of scenic delights. Fishing, boating, golf and horseback riding are among the many opportunities for recreation. Small wonder that the area has always been attractive to artists and scholars. The local museums and neighboring communities provide recreation and educational experience.
