| Volume 33 Number 5 | Stony Brook, NY | < May 2020 > |
 |
|
 |
|
Chairman's Message

TJ Gan, MD, MHS, FRCA, MBA Today marks the 25th day since Stony Brook Hospital reached its peak of over 500 COVID-19 + PUI cases. We have seen a gradual decline in the total number of COVID patients and those needing ICU care. Faculty, residents and staff are still being re-deployed to take care of COVID patients in the ICU as well as 24/7 airway teams. With the reduction in ICU patients, the ASC which was converted to ICU is now closed. The old CTICU has been converted to a non-COVID unit under the supervision of MICU staff. Our team is being re-deployed to take care of COVID patients on 11S. Though we are not ready to resume elective surgery, the perioperative team is working on a plan to get us there when we meet the various criteria mandated by the DOH. Amongst them are the availability of 30% of the hospital and ICU bed capacity from the peak, a change of fewer than 10 hospitalizations of COVID-19 patients at the hospital in the previous 10 days, as well as the availability of personnel, PPE and testing capability. I would like to thank all of you for the excellent job you are doing during this COVID-19 pandemic. Many of you have gone above and beyond your normal duties to help take care of ICU patients, most are very sick, with high mortality, and on the airway team, taking overnight calls, etc. The teamwork you have shown and the camaraderie among team members are truly amazing and I am very proud to lead Team Anesthesia as we provide the best compassionate care for the patients. Matthew, Dr. Schabel’s son, has very kindly put together a video (see below) capturing some of the moments during this pandemic. These moments reflect current everyday life in the fight against COVID-19 and attempts to capture the selfless and indomitable spirit of our Team Anesthesia family. 
|
 |
|
Pandemic Activities in the Department
James P. Dilger, PhD In this issue of SleepTalker, we feature some of the ways that members of the Department of Anesthesiology have responded to the pandemic, not only the all-important clinical care response. As you will read, teaching, research and academic clinical efforts have tackled some of the issues or have adapted in order to be able to continue. Their efforts are inspiring. This is followed by some of the artwork submitted to the Covid Young Artists Challenge. This section of SleepTalker concludes with Matthew Wang's awesome video! Thanks to everyone who contributed photos. 
|
 |
|
Research During the Pandemic



Stony Brook University News has a detailed timeline of the project development from March 28 to April 6. 
Of course, the team built it with the idea that anybody interested in the shield is free to do so and can use their design and instructions for building their own devices. They’ve launched a website which contains information for clinicians as well as full production/manufacturing/assembly plans and files. At this point the site describes the passive version, but they will upload the negative pressure version once they and the clinicians are happy with the results. If interested, people are free to contact Armen at aenikolopov_at_gmail.com for recommendations on fabrication shops that can carry out manufacture. 
|
 |
|
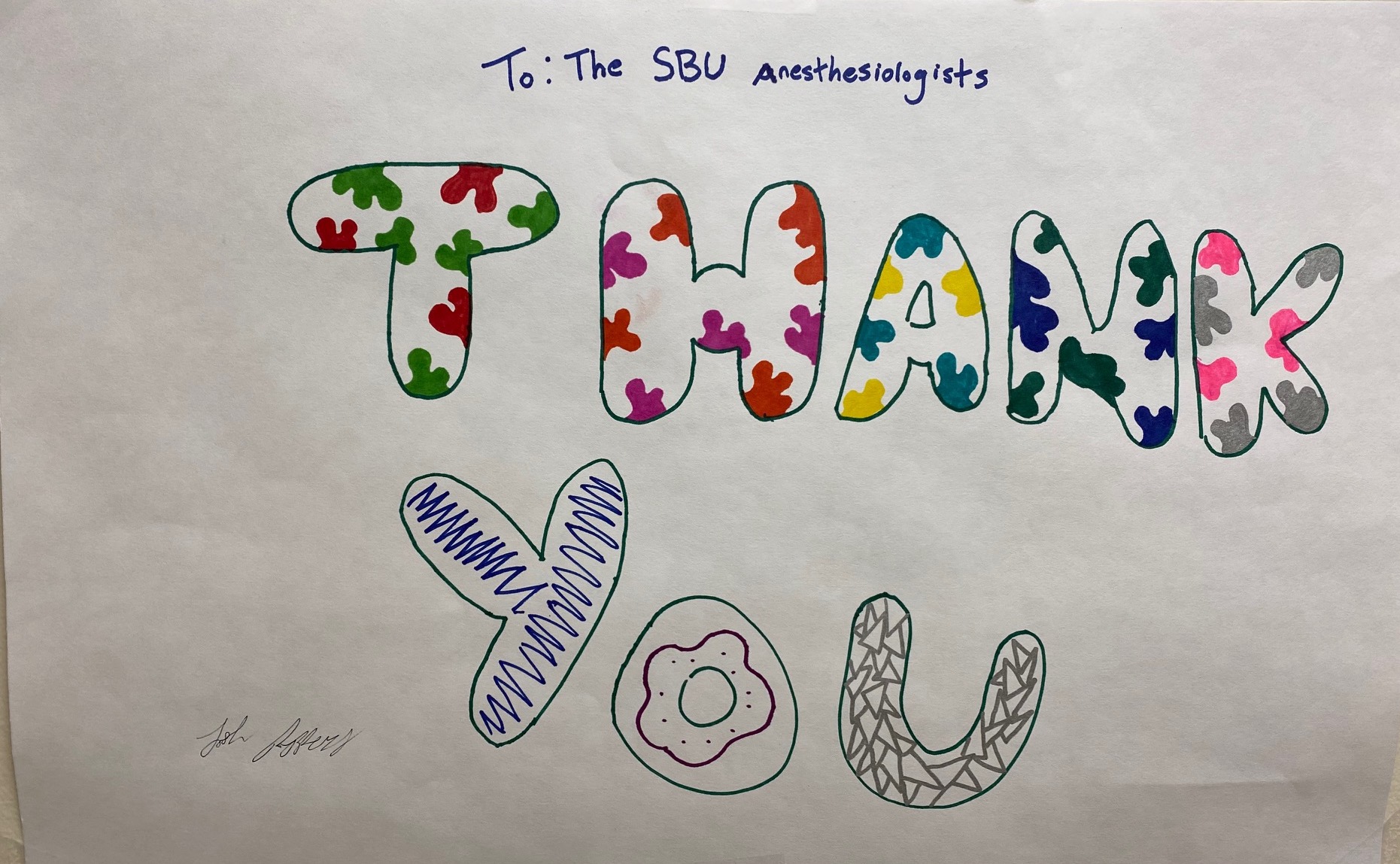
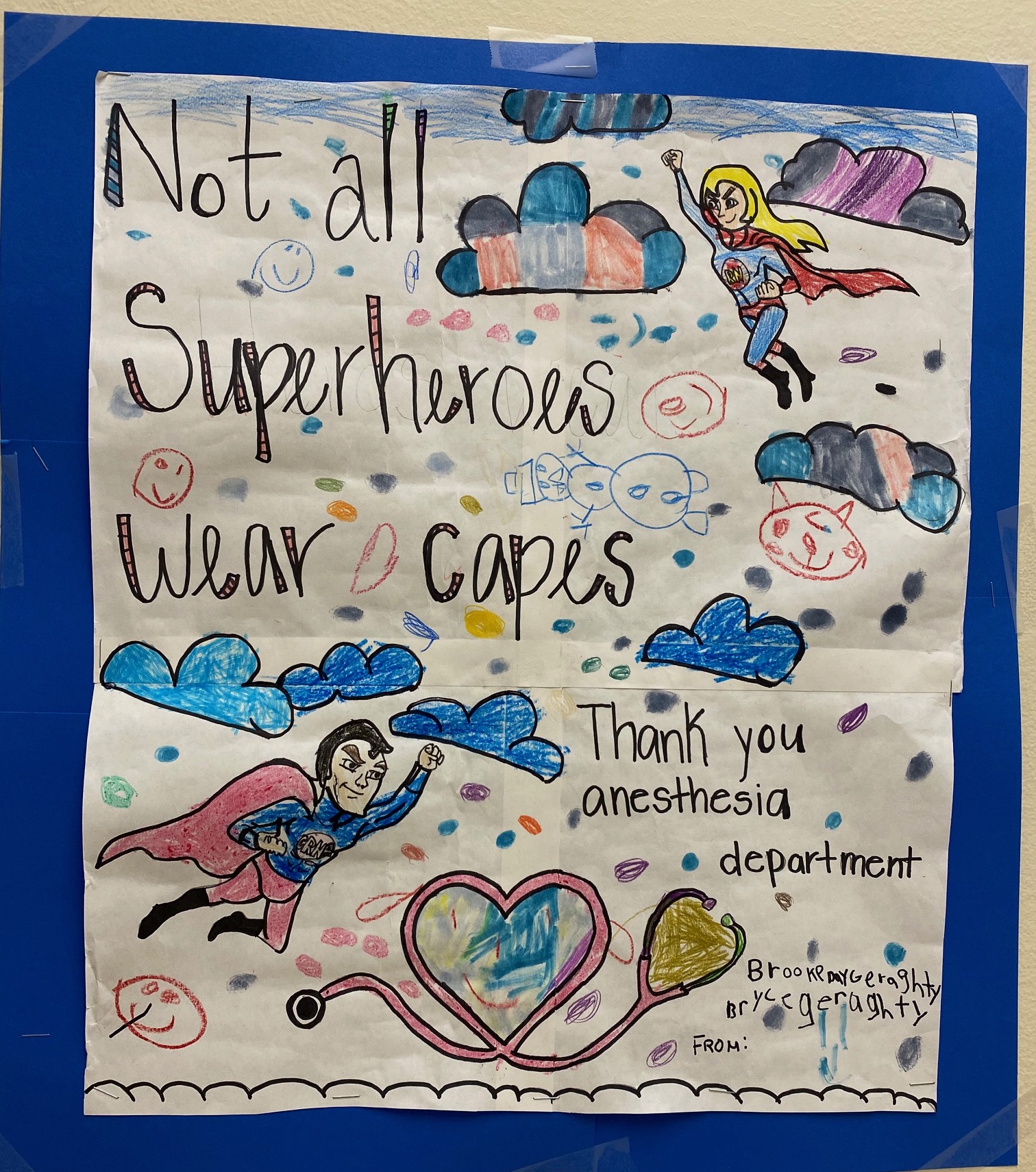
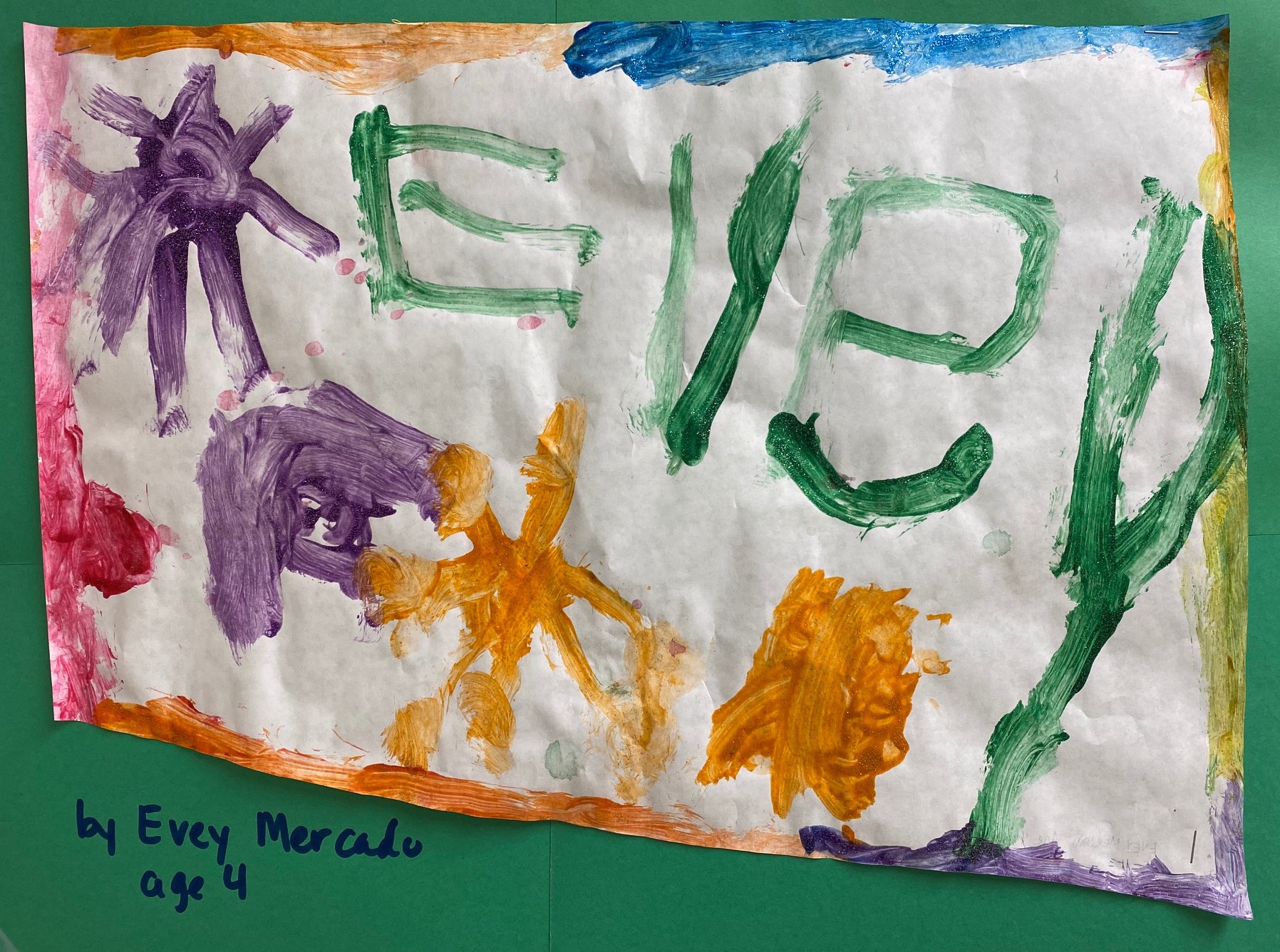
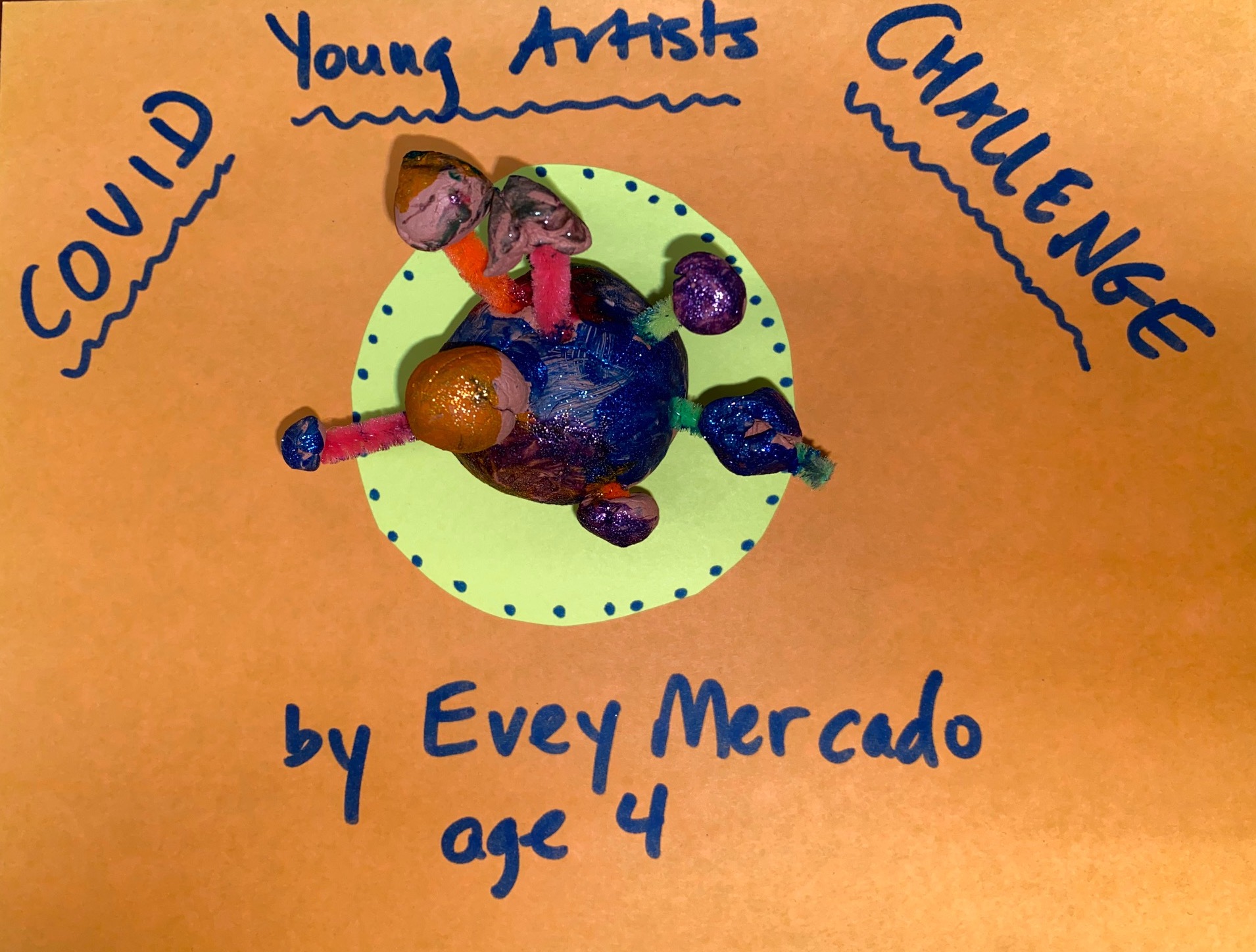
Covid Young Artists Challenge

|
 |
|
Stony Brook Anesthesiology COVID 19
Matthew Wang

|
|
New Publications

Figure from McInerney et al

|
|
Where on Campus is That?
|
|
SleepTalker, the Stony Brook Anesthesiology Newsletter is published by the Department of Anesthesiology
Stony Brook Medicine, Stony Brook, NY Tong Joo Gan, M.D., MHS, FRCA, MBA, Chairman Editorial Board: James P. Dilger, Ph.D.; Stephen A. Vitkun, M.D., M.B.A., Ph.D.; Marisa Barone-Citrano, M.A.; Ramanjot S. Kang, M.D. |