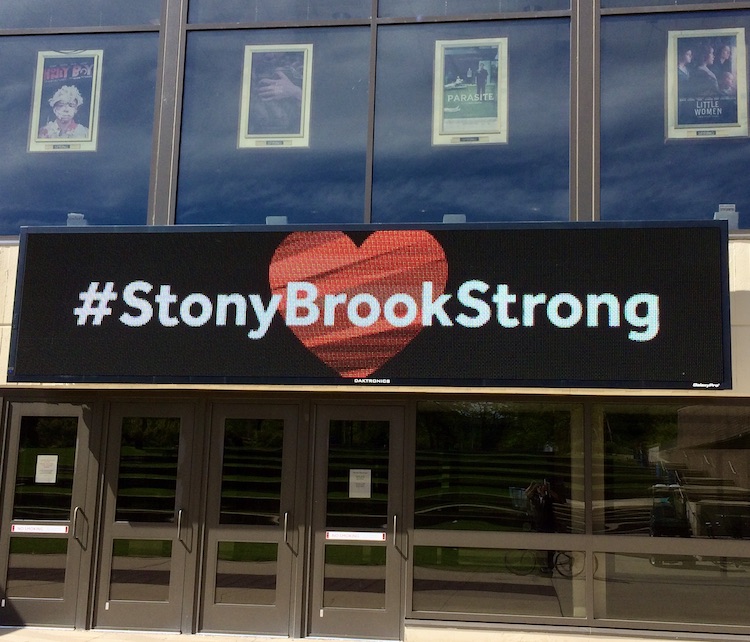
| Volume 33 Number 6 | Stony Brook, NY | < June 2020 > |
 |
|
| Covid-19 Essay | Innovation During the Pandemic | Kudos | Chief Residents 2020-21 |
| Anne Stowell Retires | Newborns | Graduations | SARAS Cancelled |
| New Publications | Photography Corner | Where is That? |
 |
|
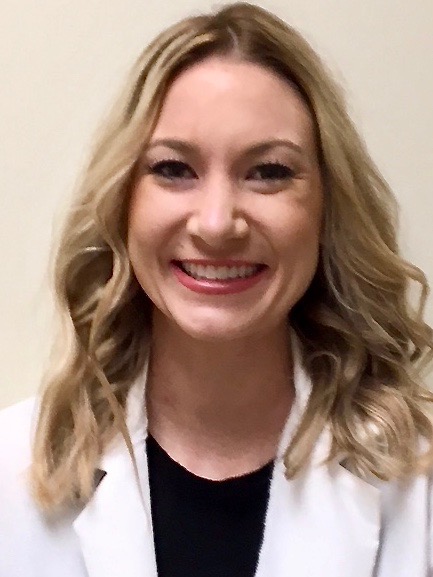
Reflections of an Ambulatory Anesthesiologist from the COVID Front Lines

Tazeen Beg, MD They are calling us the Front Liners. I never thought of us–anesthesiologists–as frontline workers until the onslaught of COVID-19. Placing an endotracheal tube in someone who is in respiratory distress is part of our job and we are doing it with commitment and passion because that is what we are trained to do. To say that it is overwhelming to be on the front lines would be an understatement. Our 600 bed, level 1 trauma center has been basically turned into a COVID-19 hospital with regular floors being converted into intensive care units. The Ambulatory Surgery Center next door is a COVID-19 ICU now that all elective surgery is cancelled. The ICUs are manned not only by Intensivists, but also physicians who never thought they would ever be required to see such patients when they were deciding on their future specialty! To be in an unfamiliar realm, out of your comfort zone, is very unnerving but a call for duty is just that. A doctor will never refuse to take care of a patient. The residents and fellows have been redeployed similarly. Even medical schools graduated their students early so that they could be put to use. This is unprecedented. Being on the COVID-19 Airway Team from the outset of this pandemic has been both a learning and reflective experience. Anesthesiology is a very high-risk specialty and brings along responsibility. We are literally supporting life every day. We put patients to sleep, but more Outpatient • Office Based • Non-Operating Room importantly, we wake them up. During this pandemic we are putting patients to sleep in order to intubate and help them breathe and rest their tired lungs. But the difference today is the uncertainty. We are not positive we can wake them up. Approximately 70-80% of patients being intubated do not make it.1 It’s brutal.
We try not to think about it too much.
We are kind of privy to the patient’s last conversations. But it doesn’t work all the time. On one of my 12-hour shifts (we do 12-hour shifts for seven days or nights straight), we were called to intubate an otherwise healthy 28-year-old on the 16th floor of the hospital. We arrived to find a young male short of breath, with a non-rebreather mask on his face texting someone on his phone. He was hot and flushed. Just before he went off to sleep, he looked at me with fear in his eyes and asked if he was going to wake up from this. Will he survive? He was tachycardic, desaturating and his labs looked dismal. I still wonder if I did the right thing with my usual reassuring nod and answer, 'of course, you will'. As we were doffing our PPE we got another call for intubation. We rushed to the ER down on the 4th floor to intubate an 80-year-old male presumed to be COVID-19 positive. We entered the room to find him talking to his wife on the phone. In between coughs and gasps of air, he was advising her to keep checking her oxygenation through pulse oximetry. She was at home, also COVID-19 positive and he was concerned. Their kids were in the city and hadn’t been able to come visit due to social distancing, he told me. This is a sad and lonely disease. It was not yet noon and we had already intubated five patients. Another 77-year-old man tried calling his wife when he found out he was going to be intubated and would not be able to talk. Yes, he actually asked me this question. His wife was somewhere outside the hospital, he said. The ‘no visitors allowed’ policy was in effect at the hospital. When he couldn’t reach her, he called his son. With trembling hands, voice fraught with anxiety, and short of breath he said, ‘I love you kiddo’. The son couldn’t comprehend the gravity of the situation, it seemed, and kept asking him questions. We waited patiently inside the negative pressure room with him. We didn’t want to rush him. This might be his last conversation with his son. A respiratory therapist walked in just as we were preparing to intubate. He introduced himself to the patient and said that his mother had just called him. She wanted our patient to know that she knew him from church and that she and her friends were all praying for him. This message was like a breath of oxygen for him, such that it brought a relaxed hint of a smile on his face. He seemed to be content with his life and stopped shaking as much. Maybe it was reassuring to know that someone up there was looking out for him. 
There is a lot of uncertainty and fear. I have seriously thought about the implications of my absence on my family, for one. Fear of death has definitely crossed the minds of all healthcare workers like me. We have had serious questions from colleagues about setting up a Living Will. Single moms in healthcare are worried about their kids' future. Elderly who live alone have no one to care for them. Life is precious. I have developed a fresh appreciation of life and can better understand its significance. Family, staying connected and taking care of your loved ones, is very important. You don't want to die alone. No one does. But people are dying alone. There is no one by their bedside for fear of contracting the illness or because hospitals are limiting the visitors. No funerals can be planned or held. The funeral homes are overcrowded and cemeteries are overwhelmed. There is a backlog of at least two weeks for provision of funeral services. Life is unpredictable. If you love someone, never forget to say it. Call your family and friends more often. Check on them. You don’t want your family member to become a statistic. The pandemic has made me and my convictions stronger. Today, I have more appreciation for my profession both as a physician and as an anesthesiologist. I have a deep satisfaction to be working during these difficult times. There is an enormous outpouring of support and kindness from the community and our families which has kept us going. It feels good to be appreciated. I may be doing something right. 
I want to think positive. I believe that with the collective efforts of doctors, scientists and policy makers along with public understanding and support, we will overcome it eventually. We need to have patience until a complete cure is found and a vaccine created. I am proud to be a part of this team as we find our way forward through today’s uncertainty, pain and fear with intelligence, resilience and perseverance. Cooperation is critical. I do hope as a society we do not go back to the so-called 'normal life' but hopefully have had time to reflect and learn valuable lessons. We need to come together not only in the region but all over the world. Maybe COVID has acted as a catalyst for a better world. Or at least I would like to think so. We will know more in the coming months. 1 Yang X, Yu Y, et al. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study. Lancet Respir Med. 2020 May;8(5):475-481. doi: 10.1016/S2213-2600(20)30079-5. Epub 2020 Feb 24 Editor's note: Dr. Beg wrote this essay for SAMBA, the Society for Ambulatory Anesthesia. She has since received requests for interviews from several news media organizations including Britain's Daily Mail. 
|
 |
|
Innovation During the Pandemic

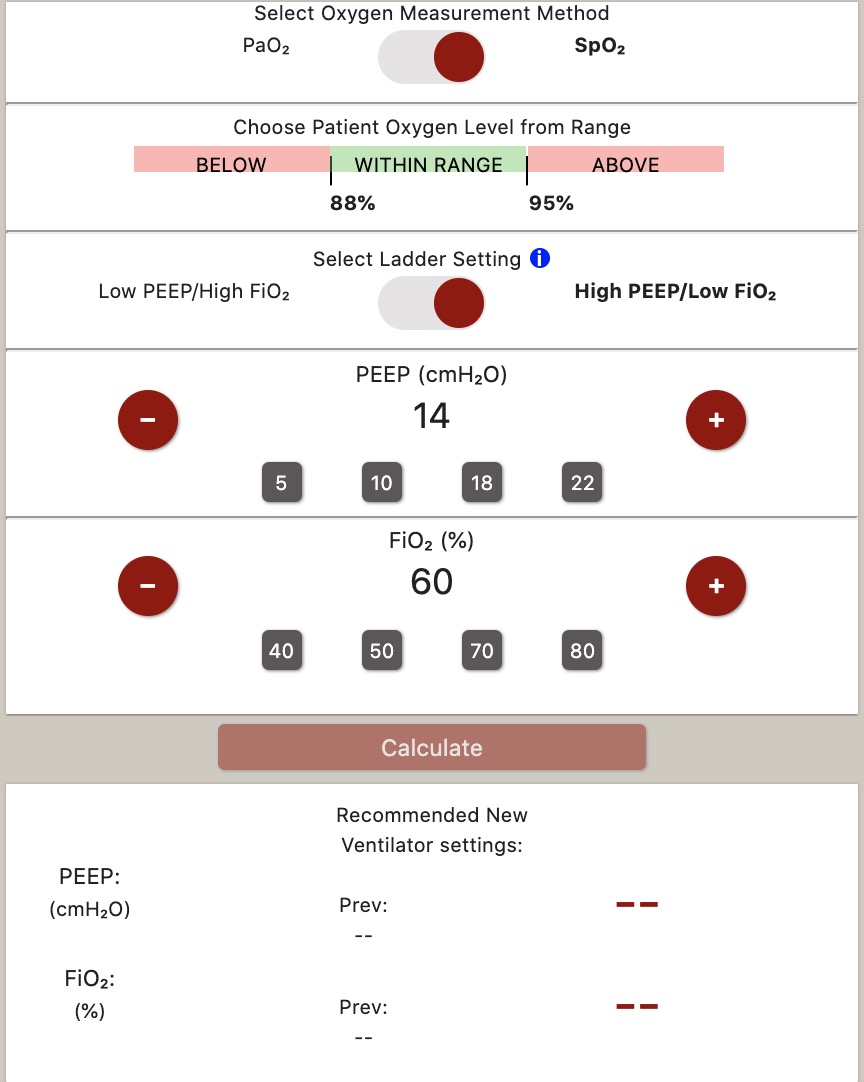
Dr. Jonathon Schwartz and colleagues from Computer Science and Biomedical Engineering created an applet, Vent, to assist in optimizing ventilator settings and anesthesia machine gas flows to target a specific oxygen concentration. It was designed during the COVID surge and was used briefly before the surge subsided. But it is ready in case there is a resurgence in the Fall. The team hopes to adapt and revise it further. Jonathon will be glad to answer any further questions about this project. 
|
|
Kudos
Dr. Srinivas Pentyala was appointed Adjunct Professor of Mechanical Engineering. This brings his total number of adjunct positions at Stony Brook University to five! The others are Orthopedics, Urology, Health Sciences, and Physiology & Biophysics. He was also invited to become a member of the National Academy of Inventors. Congratulations, Srini!


|
|
SARAS 2020 Cancelled
Srinivas Pentyala, PhD
The annual SARAS event that is organized by our department will be taking a break after 16 years of continuous programing. SARAS hosts more than 130 high school students every year exposing them to different aspects of biomedical science. More than 80 faculty and staff are involved with SARAS every year providing lectures and workshops in different areas of medicine and biology. Despite roadblocks and logistics issues SARAS was organized successfully for the past 16 years, until COVID-19 created a hard stop this year. The SARAS organizing team is hoping to come back strong to organize the 2021 event in a much bigger and brighter fashion. 

|
|
New Publications
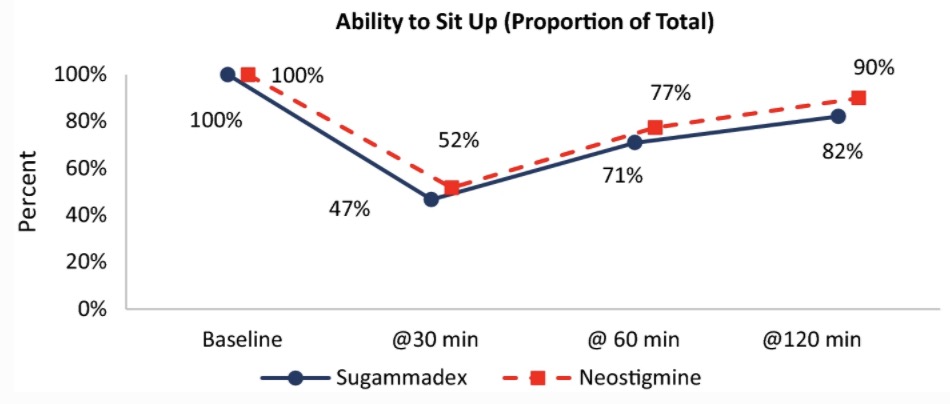
Figure from Abola et al 2020

|
|
Photography Corner
|
|
Where on Campus is That?
|
|
SleepTalker, the Stony Brook Anesthesiology Newsletter is published by the Department of Anesthesiology
Stony Brook Medicine, Stony Brook, NY Tong Joo Gan, M.D., MHS, FRCA, MBA, Chairman Editorial Board: James P. Dilger, Ph.D.; Stephen A. Vitkun, M.D., M.B.A., Ph.D.; Marisa Barone-Citrano, M.A.; Ramanjot S. Kang, M.D. |