| Volume 32 Number 6 | Stony Brook, NY | < December 2019 > |
 |
|
|
December Calendar
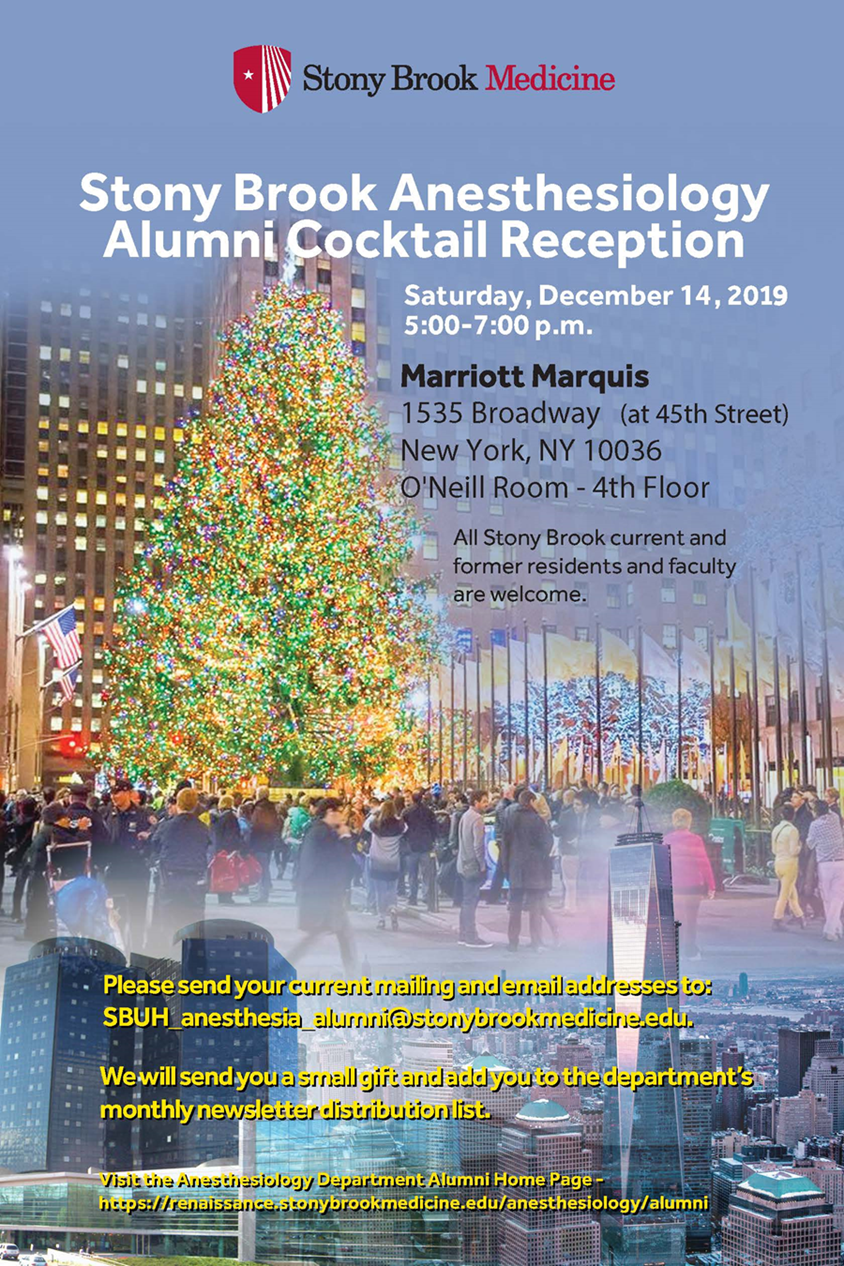
RIGHT NOW! At least, before Fri. Dec. 6. RSVP for the Holiday Party!!! Wed. Dec 4. Dr. TJ Gan will chair the Faculty meeting at 7:00 am in LH5. Wed. Dec 11. Senior Grand Rounds at 7:00 am in LH5. Wed. Dec 11. The Anesthesia Book Club will meet at 6:00 pm at Maria's Restaurant in Smithtown. Sat. Dec 14. Alumni Cocktail Reception at 5:00 pm at the Marriott Marquis Hotel in NYC. Wed. Dec 18. Dr. Adsumelli will chair the QA Committee meeting at 7:00 am in LH5. Fri. Dec 20. Annual Holiday Party at 7:00 pm at Flowerfield, St. James. 
|
|
Anesthesia Book Club
So, if you are a reader, or just would like to get out and socialize with colleagues, why not give the Book Club a try? Can't make it this month? Email Sunitha Singh and she'll put your name on the mailing list and keep you posted about future meetings/books. 
|
|
Anesthesiology News

In July, Dr. Sunitha Singh was interviewed about the poster she presented at the 2019 Annual Congress of the American Society for Enhanced Recovery. She had surveyed US hospitals about their use of ERAS in different types of surgery. More than half of hospitals reported that they had ERAS programs for colorectal, gynecology and orthopedic surgery. At the other end, fewer than 15% had ERAS programs for ENT, vascular and cardiac surgeries. The October issue, Jamie Romeiser was quoted on the feasibility studies she did on electronic capture of perioperative patient-reported outcomes. She had presented her results in two posters from the ASER meeting. She reported that nearly three-quarters of patients responded with an email and text combined approach,an extremely high compared to usual hospital surveys. Last month, Zhaosheng Jin's new systematic review and meta-analysis, presented at the IARS meeting, was discussed. His work concluded that patients undergoing TIVA with propofol had lower rates of cancer recurrence and higher rates of recurrence-free survival than those receiving a volatile anesthetics. However, there was no significant difference between groups in overall mortality. 
|
|
New Publications

|
|
Where on Campus is That?
|
|
Monthly Muscle Chillaxant

We celebrated the birthday of Ana Martinez! 
Friendsgiving Lunch! 
|
|
SleepTalker, the Stony Brook Anesthesiology Newsletter is published by the Department of Anesthesiology
Stony Brook Medicine, Stony Brook, NY Tong Joo Gan, M.D., MHS, FRCA, MBA, Chairman Editorial Board: James P. Dilger, Ph.D.; Stephen A. Vitkun, M.D., M.B.A., Ph.D.; Marisa Barone-Citrano, M.A.; Ramanjot S. Kang, M.D. |