| Volume 33 Number 1 | Stony Brook, NY | < January 2020 > |
 |
|
|
Visiting Professor, Dr. Maxime Cannesson
James P. Dilger, PhD Hailing from UCLA Department of Anesthesiology & Perioperative Medicine, our Visiting Professor this month is Maxime Cannesson, MD, PhD. Dr. Cannesson wears several hats in his department: Professor of Clinical Anesthesiology, Vice Chair for Perioperative Medicine, Director of Clinical Research, and Vice Chair for Research. His research specialty is Perioperative Medicine. Dr. Cannesson received his MD from Denis Diderot University, Saint Louis Hospital in Paris, France. HIs residency in anesthesiology was at Claude Bernard University, Hospices Civils de Lyon Medical Center in Lyon, France. Subsequently, he received a PhD in Cardiovascular Physiology from Claude Bernard University. In 2004, he came to the US and did a fellowship at the University of Pittsburgh Medical Center. Dr. Cannesson's research is focused on phenomics, the study of the interaction of genes and the environment, and how it can shape the management of critically ill patients. His group uses computing and informatics to develop novel monitoring systems, and to develop predictive physiological tools. Dr. Cannesson will be at Stony Brook on Tuesday, January 21 when he will speak to the residents at 5 pm and on Wednesday, January 22 when he will address the department at 7:00 am. Welcome to Stony Brook Dr. Cannesson! 
|
|
Chief's Corner - General Anesthesia Division
Trauma Center at Stony Brook Daryn Moller, MD 
What does it mean to be a Trauma Center? Trauma Centers are categorized in Levels 1 through 4; a Level 1 Trauma Center has the most resources and a level 4 the least. In areas of sparse resources such as a rural setting, level 4 facilities provide stabilization of injured patients and expedited transfer to a facility that can provide definitive care. Level 4 trauma facilities may only be staffed by a mid-level provider such a as Physician Assistant or Nurse Practitioner where Level 3 trauma facilities are capable of providing some rudimentary damage control surgical procedures. Both Level 3 & 4 Trauma Centers lack many resources that we take for granted, yet they are a vital part of a functional trauma system network. It allows the most rapid access to care possible, regardless of the geographic location the injury occurred. Both Level 1 and Level 2 centers have a breadth of resources to allow for all aspects of definitive care of the injured patient such as neurosurgery, complex orthopedics and cardiothoracic surgery. Level 2 centers may be either private or academic centers, but frequently lack specialized resources such as the capability to replant digits, oral-maxillofacial or ophthalmologic services. In both Level 1 & 2 Trauma Centers, resources must be available in a timely fashion to the injured patient: An trauma surgeon must be available at the bedside within 15 minutes. Ancillary services such as neurosurgery, interventional radiology must also be available within 30 minutes of activation. (Please remember to sign and date the Trauma flow sheet for every Code T, it documents the timely presence of Anesthesia Services.) 
CODE T
• Cardiac Arrest after Trauma
• Airway obstruction or compromise • Confirmed SBP < 90 mm Hg at any time • Advanced airway requirement from the scene • Penetrating injury to head/neck/chest or abdomen • GCS <= 8 with a presumed Trauma mechanism • Suspect Spinal Cord injury • Traumatic Amputation above wrist or ankle • Inter-Hospital Transfer receiving blood/pressors to maintain vital signs Trauma Alert
• Penetrating injury of extremity with concern for Vascular Injury
• Femur/ 2 or more long bone fractures • Fall > 20 feet • Burns > 15% BSA • Amputation below wrist or ankle • Pedestrian struck > 15 mph • Motorcycle crash > 20 mph or separation of rider from bike • GCS 9-12 with presumed Trauma mechanism • >20 weeks pregnant with abdominal pain or potential significant injury mechanism • Interhospital transfer with intracranial injury • Patients with reduced physiologic reserve what may have intra-abdominal or thoracic injury 
All behind the scenes as well as direct clinical activities are monitored and reported to Trauma Quality Improvement Program that tracks a programs performance in comparison to its peers. This risk adjusted data base reports back to each of the institutions how they are doing in comparison to their peer group. Stony Brook has received a “better than expected” response for 30 day trauma mortality for at least the past year. So when someone sees a hip fracture for a pre-operative block or sees the same patient in the late afternoon as an add on case, please understand that there is a reason behind it all; as members of the trauma group, we are all trying to provide the most timely and optimal care of the injured patient. 
|
|
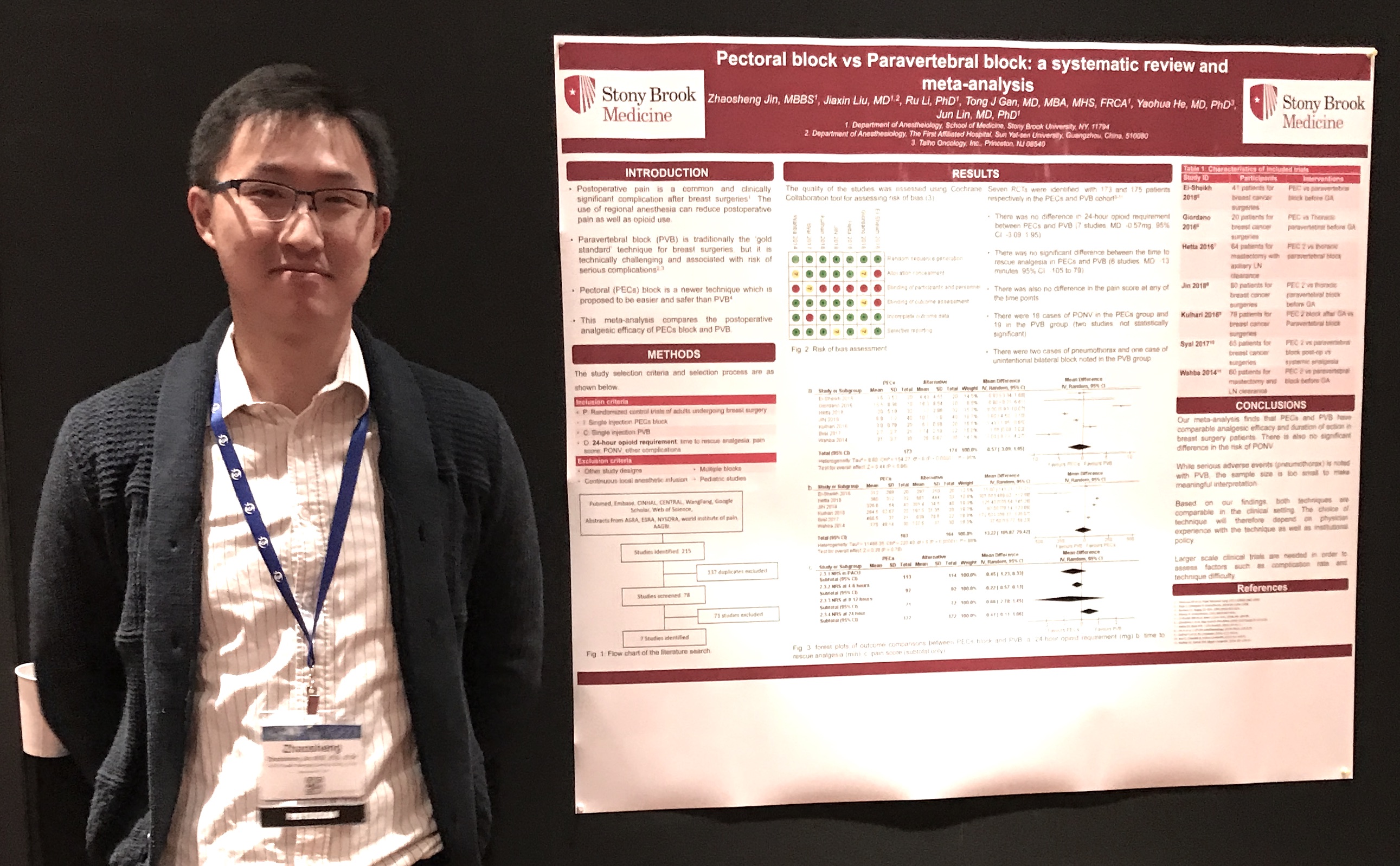
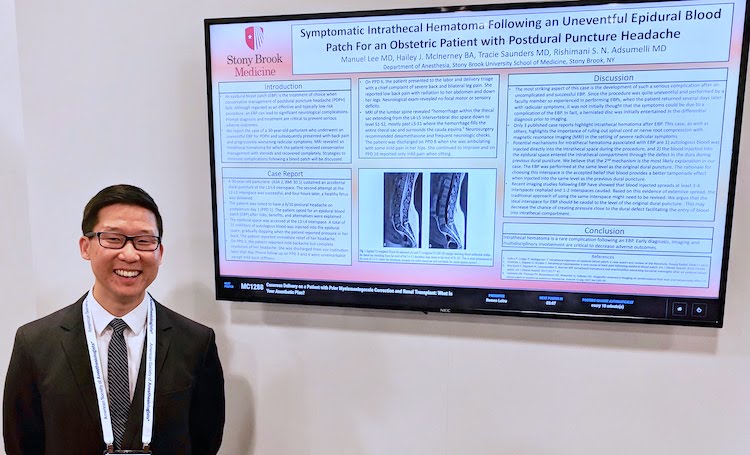
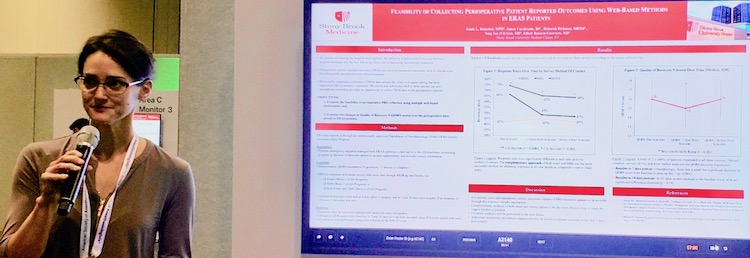
Stony Brook Anesthesiology at PGA 2019
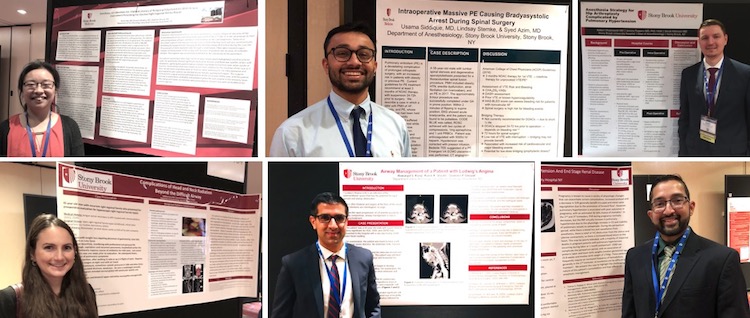
Residents Dr. Shuran Ma, Dr. Usama Siddique, Dr. Robert Chojnowski, Dr. Kathleen Cervo, Dr. Ramanjot Kang, and Dr. Ravi Shah at their PGA posters. Click here for more photos from the PGA meeting. 
|
|
Alumni Reception

We had a record turnout of more than 70 at the Alumni Reception this year! This is probably due to the relocation of the event to the PGA hotel. Click here for more pictures from the evening. 
|
|
Holiday Party

|
|
New Publications

|
|
Where on Campus is That?
|
|
Monthly Muscle Chillaxant
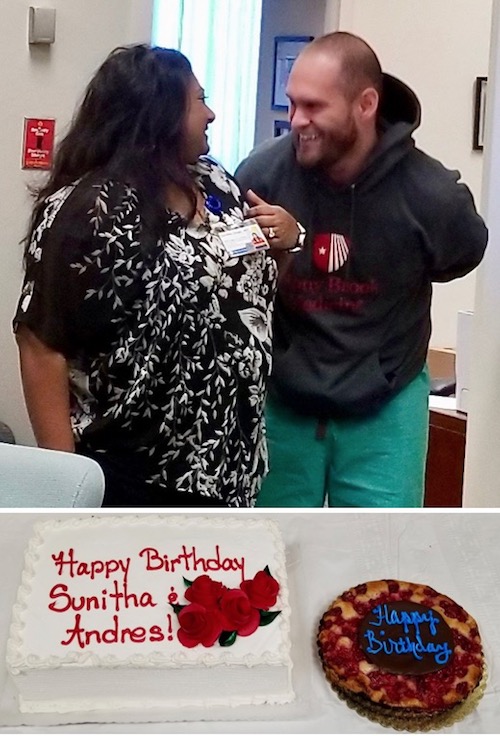
We celebrated the birthdays of Sunitha Singh and Andres Perez 

To get into practice for eating extra goodies this season, we had a Holiday Brunch! Some of us even accepted the challenge of wearing an ugly sweater for the occasion! Click here for more photos of the brunch. 
|
|
SleepTalker, the Stony Brook Anesthesiology Newsletter is published by the Department of Anesthesiology
Stony Brook Medicine, Stony Brook, NY Tong Joo Gan, M.D., MHS, FRCA, MBA, Chairman Editorial Board: James P. Dilger, Ph.D.; Stephen A. Vitkun, M.D., M.B.A., Ph.D.; Marisa Barone-Citrano, M.A.; Ramanjot S. Kang, M.D. |