
| Volume 37 Number 1 | Stony Brook, NY | < January 2022 > |
 |
 |
| Dr. Corrado | Dr. Probst | STARS | Holiday Party |
| PGA 2021 | Holiday Call Teams | What's Happening Alumni? | Peek Behind the Pub |
| ASRA Meeting | New Publications | Where on Campus is That? | Monthly Muscle Chillaxant |
|
Dr. Corrado Named Medical Director of Perioperative Services
Tong J (TJ) Gan, MD, MBA, MHS, FRCA 
Dr. Corrado is very well-known to Stony Brook. After completing his undergraduate and graduate studies at St. John’s University, his 17-year career began at Stony Brook, where he earned his medical degree, interned in the Department of Medicine and completed his training in Anesthesiology. In 2009, he joined our department as an Assistant Professor and Attending Anesthesiologist. Over the years, Dr. Corrado has taken on many key roles in our department, including Resident Education Coordinator for the Neuroanesthesia Division; Ear, Nose and Throat Sub Division Director; Director of the MOCA Simulation Program; Operating Room Coordinator; Assistant Clinical Director of the PACU; and Chief Operating Room Coordinator. More recently, Dr. Corrado has led the OR Throughput and Efficiency Project. Within a short timeframe, his team was able to increase the on-time starts from a three-year average of 37% to over 77% percent. This placed Stony Brook in the top quartile and near the top decile for comparable institutions. Dr. Corrado’s leadership in this effort has created a collegial, perioperative environment among all the stakeholders, including surgeons, anesthesiologists, nursing, and staff. The next focus of his team will be to improve other areas of efficiency, including the operating room case turnovers. I am confident that the collaborative culture he has helped to cultivate will be instrumental in the continued success of his team. In his new role, he will be assisted by Dr. Stephen Probst, the new Associate Medical Director of Perioperative Services. Both Drs. Corrado and Probst have been working closely together in the management of perioperative services and I expect to have a seamless transition in the change of leadership. I would like to thank Dr. Ken Rosenfeld for his enormous contribution to Stony Brook Medicine, which spans over 30 years. He started as a resident in our department, then faculty member, interim department chair, and president of the Medical Board, to name a few of his many roles. He is well known to all of us at Stony Brook and we will miss his dedication to the institution and his sense of humor. I wish him great success as he embarks on a new chapter in his career. Please join me in welcoming Dr. Corrado to his new role. |
|
Dr. Probst Named Associate Medical Director of Perioperative Services
Tong J (TJ) Gan, MD, MBA, MHS, FRCA
Dr. Probst received his B.S. in biology/chemistry from Mount St. Mary College in Newburgh, New York and his M.D. from Stony Brook. He completed a residency program in Anesthesiology here at Stony Brook. Soon after, he joined our department as an Assistant Professor in 2008. Over the years, Dr. Probst has held progressively important roles. In 2010, a new section within the Neuroanesthesia and ENT anesthesia division was created to address the increasing number of interventional neuroradiology and neurosurgery cases at Stony Brook. Dr. Probst’s calm demeanor and reputation as a skilled clinician made him the ideal person to lead the new section. Not surprisingly, two years later, he was appointed the Chief of the Neuroanesthesia and ENT Anesthesia Division. In 2013, he became one of the Operating Room Clinical Coordinators. During this time, he created a dedicated cerebrovascular anesthesia on-call team. His significant leadership and managerial skills led to his recent appointment as the Anesthesiology Department’s Director of Clinical Affairs. In addition to being an excellent clinician, Dr. Probst has excelled as an educator. He was an integral part of our Basics of Anesthesia lectures and developed the curriculum for neuroanesthesia. He also developed a mini fellowship for residents in the cerebrovascular discipline. He has served on numerous departmental and hospital committees, including the University Hospital Medical Board and our department’s executive committee. Please join me in welcoming Dr. Probst to this new role. |
|
STARS: STaff Appreciation and Recognition

Jeremy S. Poppers, MD PhD, FASE I want to highlight the outstanding efforts of Zach Adams, CRNA in a case. We had a 94yo patient undergoing a micra PPM in EP lab. The case was running smoothly until the patient suddenly became hemodynamically unstable (SBP 140s --> 60s). Zach immediately called me to alert me to the situation and sprang into action. In a matter of minutes, he had addressed the hemodynamics pharmacologically and expertly placed a large bore IV and an aline. His thought process was clear, definitive and efficient, as were the actions he took. There was no panic, hesitation or perseveration. I was very impressed and the patient is alive and well as a direct result of Zach's phenomenal care. Patient comments about our Ambulatory Surgery Center staff are compiled from the Press Ganey questionnaires by Marisa Barone-Citrano, MA Everyone was wonderful, the anesthesiologist was perfect, had an issue previously with someone else. Dr. Syed Shah was wonderful hope to get him again at your next visit. |
|
Holiday Party 2021
|
|
PGA 2021

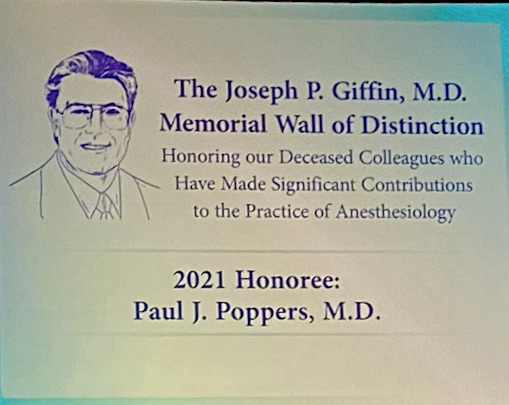
The Founding Chairman of the Department of Anesthesiology, Dr. Paul J. Poppers, has been awarded the 2021 Joseph P. Giffin Memorial Wall of Distinction Honor. This Honor from the New York State Society of Anesthesiologists is posthumously bestowed on an anesthesiologist who has made significant contributions to the practice of anesthesiology. Dr. Poppers was Chairman of the Department from 1979 to 1999. He passed away in June 2019. Abstracts
Costa A, Chandran L, Schabel J, Abola R, Fischel J. Practice Habits and Data Analytics in Anesthesiology Resident Education
Medically Challenging Cases
Li R, Jin Z, Lin J. Combined general/epidural anesthesia vs general anesthesia on the postoperative inflammation or stress response: a systemic review and meta-analysis Jin Z, Li R, Lin J. Intravenous vs volatile anesthesia and colorectal cancer surgery outcome - a systematic review and meta-analysis 
Bindelglass A, Richman D, Cecchetto K. Perioperative Approach to a Patient with Hereditary Amyloidosis Kang R, Shuaib K, Parikh S, Desai A. Epidural Analgesia For Chemical Pleurodesis Kang RS, Mena S, Nguyen C, Kogan A. Peripheral Nerve Catheters For Post-Amputation Pain Control Kozlowski P, Shafai A, Wu D, Kaushal A. Exacerbation Of Complex Regional Pain Syndrome After COVID-19 Vaccination Lin G, Kang RS, Oleszak S. Laryngeal Stenosis After Inhalational Injury: Airway Management and a Review of the Literature Mathew A, Figueroa C, Oleszak S, Atkinson D. The Supraglottic Airway Device As An Intubation Conduit Mathew A, Watson E, Nguyen V, Tateosian V. Airway Challenges In a Neonate With Congenital Epulis Mena S, Nguyen C, Kang R, Oleszak S. The Anticipated Difficult Airway: Tracheal Stenosis After COVID-19 Infection Mena S, Parikh S, Desai A. Neuraxial Analgesia For A Sacral Decubitus Ulcer Mena S, Poppers J, Zabirowicz E. Severe Mitral Valve Regurgitation After Tricuspid Valve Replacement Seiter C, Parikh S, Oleszak SP. An Aggressive Endobronchial Tumor Necessitating Unconventional Airway Management Shafai A, Angelo T, Landman U, Giordano M. Anesthetic Management Of A Parturient With Segawa Syndrome Shuaib K, Kang RS, Bennici L. A Pediatric Patient With Erythromelalgia Zhang K, Xiao A, Richman D. Anesthetic Management of Intrabronchial Valves
Kang RS, Alam S, Bracero L, Figueroa C, Kant I, Kim B, Mathew A, Shuaib K, Watson E, Xiao A, Gidicsin C, Romeiser J, Costa A, Bennett-Guerrero E. AIRWAY: Improving Preparation for Floor Intubations
Daoud B, Goodman SR. Maternal Cardiopulmonary Resuscitation
Scientific Panels
Bergese SD. The Long & Short Impact of Opioids Costa A. Robotic Partial Nephrectomy Costa A, Factor M. Managing Errors: How to Identify & Evaluate Wrong-Route Medication Error on Labor & Delivery Beg T. Vaping and E-Cigarettes: Anesthetic Consideration Daoud B. Maternal Cardiopulmonary Resuscitation
Gupta A. 21st Annual Bragging Contest
Spotlight Sessions
Moore RP. Pediatric Ambulatory Anesthesia: Leveraging the literature to develop and evaluate patient-centered ambulatory care for children
Moore RP. Pediatric Ambulatory Anesthesia: Leveraging the literature to develop and evaluate patient-centered ambulatory care for children
Workshops
Bergese SD. Improving Outcomes in the Geriatric Patient - Delirium Prevention and Treatment Costa A. Postoperative Nausea and Vomiting: Practice Guideline Update Moller D. Anatomy of an Error Nada E, Gan TJ. The Concept of Enhanced Recovery After Surgery (ERAS) Richman D. ACLS/PALS Update 2021
Oleszak SP, Vitkun SA. Difficult Airway Management
Chair and Moderator
Vitkun SA. Advanced Cardiac Life-Support (ACLS)
Richman D. Co-Chair of the Spotlight Session Committee
Richman D. The Covid 19 survivor and Anesthesia Implications (Moderator) |
|
Holiday Call Teams
Ramanjot S. Kang, MD

Thanks to the Call Teams who keep the department going during Christmas and New Years! |
|
What's Happening Alumni?
SleepTalker is emailed to some 200 alums (faculty, residents and staff) each month. So, you know about us, but we don't know about you! We are starting a "Life After SB Anesthesia" column and would love to hear from you! Tell us your story or share a memory in the form of prose, poetry, and/or photos. Thanks to Dr. Deborah Richman for suggesting this! Thanks to Dr. Joy Schabel, the department's Residency Program webpage has testimonials from former residents. Former residents who would like to support our recruitment efforts can send their paean to Joy directly. |
|
A Peek Behind the Publication
Yang NJ, Isensee J, Neel DV, Quadros AU, Zhang HB, Lauzadis J, Liu SM, Shiers S, Belu A, Palan S, Marlin S, Maignel J, Kennedy-Curran A, Tong VS, Moayeri M, Röderer P, Nitzsche A, Lu M, Pentelute BL, Brüstle O, Tripathi V, Foster KA, Price TJ, Collier RJ, Leppla SH, Puopolo M, Bean BP, Cunha TM, Hucho T, Chiu IM. Anthrax toxins regulate pain signaling and can deliver molecular cargoes into ANTXR2+ DRG sensory neurons. Nat Neurosci. 2021 Dec 20 Michelino Puopolo, PhD 
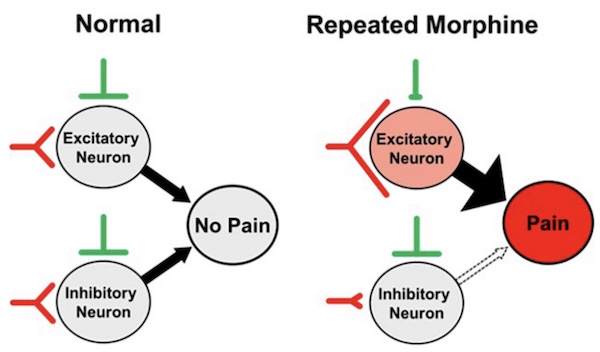
It is well known that many naturally occurring toxins from spiders and marine snails bind tightly to ion channels expressed in nociceptors to reduce their excitability and/or synaptic transmission. The final effect is to down regulate pain signals to the dorsal horn spinal cord and reduce pain. In contrast, knowledge of the direct interaction of bacterial toxins with nociceptors to modulate their excitability and pain signals is limited. It is known that infection with some types of bacteria activate nociceptors to produce pain and coughing. Other microbes appear to silence pain. The laboratory of Isaac Chiu at the Harvard Medical School showed that dorsal root ganglia neurons (DRGs) containing the NaV1.8 sodium channel and the actin-binding protein advillin, express the ANTXR2 receptor, the high-affinity receptor for anthrax toxin. Because NaV1.8+ and Advillin+ DRGs are enriched with nociceptors, Chiu wondered whether the anthrax toxin can modulate the excitability of nociceptors and pain signals. The anthrax toxin is composed of three components: the protective antigen (PA), which binds to ANTXR2, and the protein cargoes edema factor (EF) and lethal factor (LF). The initial in vivo experiments carried out by Chiu’s laboratory using several mouse models of pain proved that intrathecal administration of edema toxin (ET (PA + EF)) targeted NaV1.8+ and Advillin+ DRGs and induced analgesia. 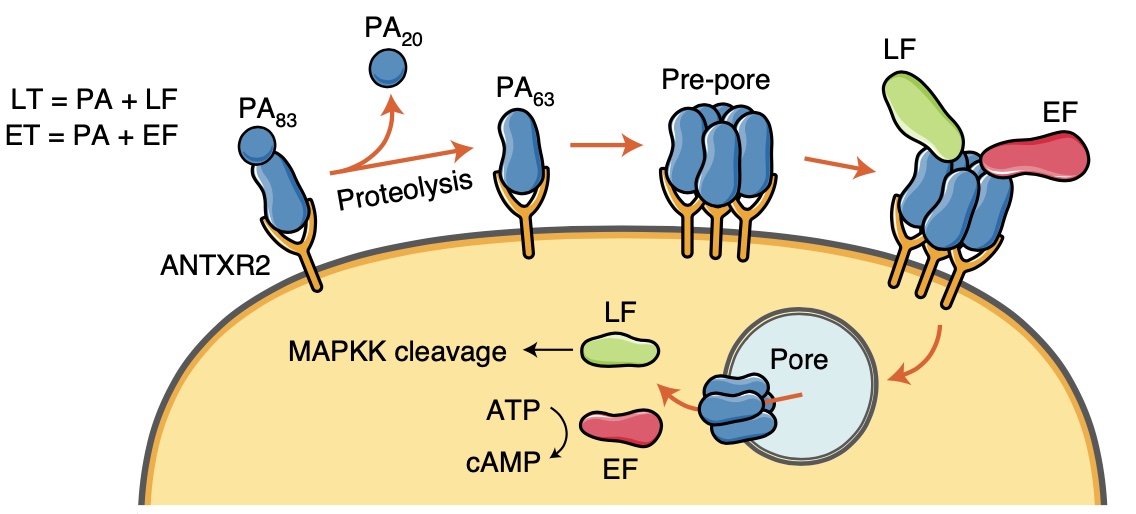
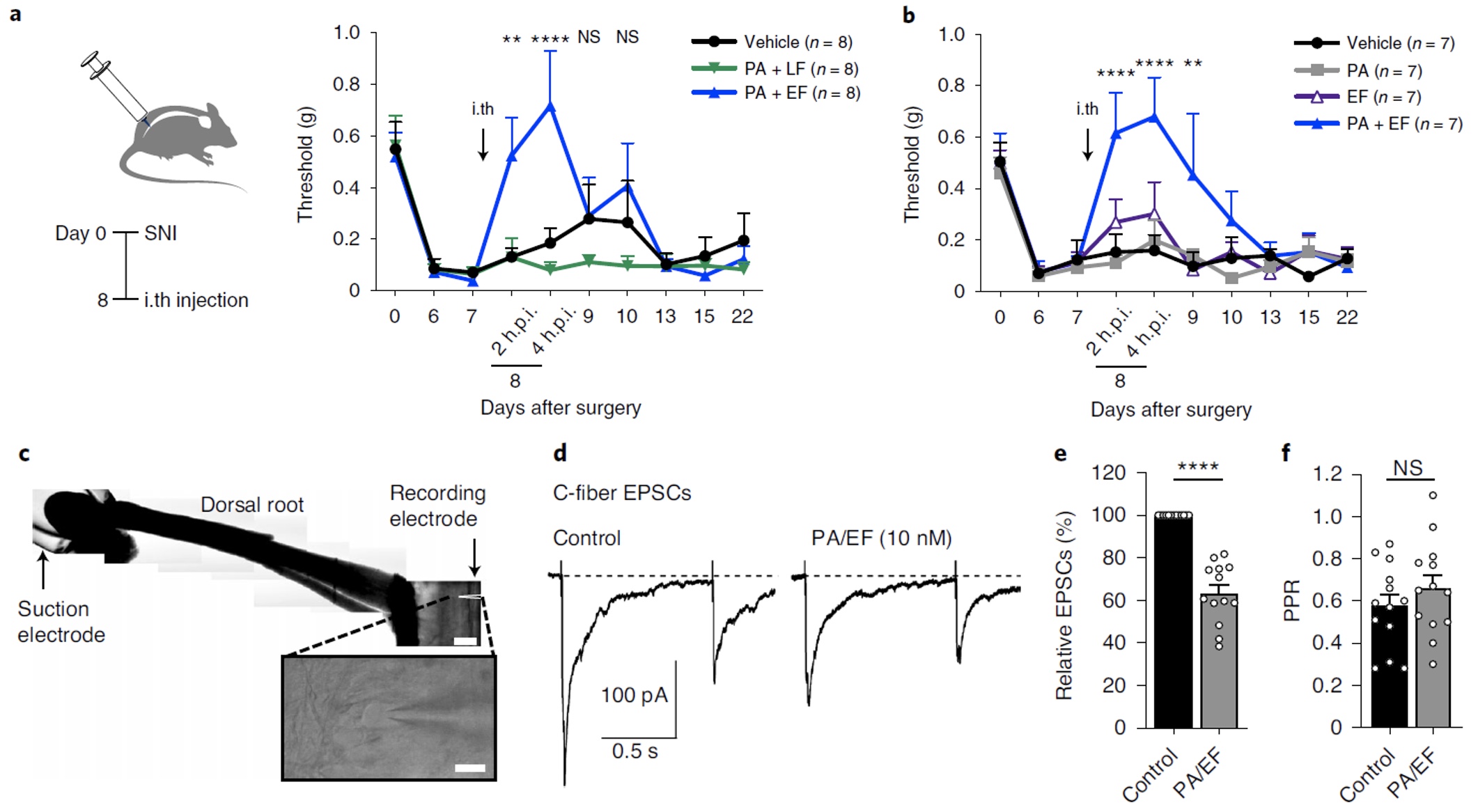
Anthrax ET silences pain in mouse models of neuropathic pain. a, Mechanical sensitivities in SNI mice injected intrathecally with vehicle, LT (2 μg of PA + 2 μg of LF) or ET (2 μg of PA + 2 μg of EF) (n = 8 mice per group). *Comparison of vehicle and ET groups. b, Mechanical sensitivities in SNI mice injected intrathecally with vehicle, PA (2 μg), EF (2 μg) or ET (2 μg of PA + 2 μg of EF) (n = 7 mice per group). *Comparison of vehicle and ET groups. c, Representative horizontal spinal cord slice preparation with the attached L4 dorsal root and a lamina I neuron (inset). Scale bar, 500 μm and 20 μm (inset). d, C-fiber EPSCs elicited in a lamina I neuron by stimulation of the L4 dorsal root (paired 400-μA stimuli at a 1-s interval). The measured conduction velocity was 0.7 m s−1, consistent with C-fiber activation. e,f, Collected results (n = 13 cells). e, Application of ET (10 nM PA + 10 nM EF) reduced the first EPSC by 37% ± 4%. f, No significant changes observed in the paired-pulse ratio (PPR). |
|
ASRA Meeting

|
|
New Publications
|
|
Monthly Muscle Chillaxant
We celebrated the birthdays of Ayesha Khan and Sunitha Singh! Best wishes! |
|
SleepTalker, the Stony Brook Anesthesiology Newsletter is published by the Department of Anesthesiology
Stony Brook Medicine, Stony Brook, NY Tong Joo Gan, M.D., MHS, FRCA, MBA, Chairman Editorial Board: James P. Dilger, Ph.D.; Stephen A. Vitkun, M.D., M.B.A., Ph.D.; Marisa Barone-Citrano, M.A.; Ramanjot S. Kang, M.D. |



